Imunologia
Aged 40+ With Diabetes Hit Badly by COVID-19, Should Be Vaccine Priority

People with type 2 diabetes as young as 40 years of age face a disproportionately increased risk of dying from COVID-19 infection, indicates a UK analysis of three large-scale datasets that shines a light on the need to prioritize vaccinations in younger vulnerable patient groups.
The research was published February 8 in the journal Diabetologia.
The majority of European countries have prioritized COVID-19 vaccinations for people with type 2 diabetes, but typically only at age 50 and older. However, the data from the current study suggest that this age limit should be lowered.
“It’s important to remember the risk to middle-aged people with diabetes of dying from COVID-19 is very low in absolute terms compared with the elderly,” said lead researcher Andrew P. McGovern, MD, of Royal Devon & Exeter Hospital, Exeter, United Kingdom, in a press release from his institution.
However, he said that “strategies to define priority groups for vaccination must consider the disproportionate relative risk of COVID-19 mortality in middle-aged people with type 2 diabetes whose COVID-19 risk is already elevated by their age.”
McGovern told Medscape Medical News that the magnitude of the effect of type 2 diabetes on COVID-19 deaths “is really what’s surprising” about these new findings, and “not what you would expect.”
He said it is therefore crucial that people with diabetes are put “into the queue” for the vaccine “in the right place, and obviously in countries where the vaccine rollout will be slower, it is more important.”
Bridget Turner, director of policy campaigns and improvement at Diabetes UK, which funded the study, said the results give “important new insights into how much type 2 diabetes adds to the overall risk of dying from coronavirus at different ages, particularly the additional risk that the condition adds in middle-age.”https://c275ced267b81d32d592c3471da53348.safeframe.googlesyndication.com/safeframe/1-0-37/html/container.html
“The UK has made good progress on prioritizing those who are most vulnerable for vaccination, which includes all adults with diabetes,” she added in the press release, “but we need to continue to work at pace to identify and protect those individuals at higher risk.”
Relationship Between COVID Death and Diabetes Is Complex
The authors note that the relationship between COVID-19-related mortality and type 2 diabetes is not simply an “additive effect of diabetes and age-related risk” but appears to be a “more complex” association, with a “disproportionately higher excess relative mortality risk in younger people with diabetes.”
To investigate this, they examined data from two UK population-based studies that had previously reported age-specific hazard ratios for COVID-19 mortality associated with diabetes:
- OpenSAFELY, which included 17.2 million people, of whom 8.8% had diabetes, and had an overall 90-day mortality rate of 0.06%
- QCOVID, comprising 6 million individuals, of whom 7% had diabetes, and had an overall 97-day mortality rate of 0.07%.
The team also looked at data on type 2 diabetes patients with severe COVID-19 from the COVID-19 Hospitalisation in England Surveillance System (CHESS), which contained 19,256 patients admitted to critical care in England, of whom 18.3% had diabetes.
The 30-day in-hospital mortality rate in this study was 26.4%.
They translated the mortality hazard ratios associated with COVID-19 infection in people with diabetes into a “COVID-age,” which equates to the additional years of “death risk” added to an individual’s chronological age if diabetes is present.https://c275ced267b81d32d592c3471da53348.safeframe.googlesyndication.com/safeframe/1-0-37/html/container.html
Taking the QCOVID dataset as an example, the results showed that the “COVID-age” associated with diabetes for someone aged 40 years was 20.4 years; that would indicate that their “mortality risk [for COVID-19] is similar to that of a 60-year-old person without diabetes.”
The impact of diabetes on the COVID-19 death risk decreased with increasing age, such that a diabetes patient aged 50 years had a COVID-age of 16.4 years. This fell to 12.1 years in someone aged 60, and 8.1 years in someone 70 years of age, which means the latter has the same risk of death from COVID-19 as someone without diabetes who is 78.
Similar results were obtained when the team looked at data from the OpenSAFELY study.
But when they looked at the effect of diabetes on COVID-19 mortality risk in the CHESS dataset, it was less pronounced.
Just Looking at Diabetes Is Oversimplistic, but It’s an Easy Marker for Vaccination
The researchers acknowledge that “considering only age and diabetes status when assessing COVID-19-associated risks…is an oversimplification,” as factors such as body mass index (BMI), diabetes duration, and glycemic control are also known to play a role.
However, they say consideration of these factors is “not practical for population-level vaccine rollout.”
“The time-critical nature of population COVID-19 vaccination necessitates pragmatic group-level prioritization, which is the approach initiated by governments thus far,” the team concludes.
This study was supported by Diabetes UK. Study author John M. Dennis is supported by an Independent Fellowship funded by Research England’s Expanding Excellence in England (E3) fund and by the NIHR Exeter Clinical Research Facility. McGovern is supported by the NIHR Exeter Clinical Research Facility.
Diabetologia. Published online February 8, 2021. Full text
Medscape Medical News © 2021
Cite this: Aged 40+ With Diabetes Hit Badly by COVID-19, Should Be Vaccine Priority – Medscape – Feb 15, 2021.TOP PICKS FOR YOU
#Rectocolite hémorragique (RCH): mise à disposition de Stelara®, 1er inhibiteur des interleukines 12 et 23

France — Après plusieurs indications en dermatologie et rhumatologie (psoriasis et rhumatisme psoriasique) depuis 2009 et une 1ère indication en gastro-entérologie avec la maladie de Crohn en 2018, Stelara® (ustekinumab, Janssen) est désormais disponible dans la rectocolite hémorragique [1].
Nouveau mécanisme dans la RCH
Stelara® est le premier inhibiteur d’interleukines (IL), ciblant les 12 et 23, à obtenir une autorisation de mise sur le marché dans la rectocolite hémorragique, une maladie inflammatoire chronique de l’intestin (MICI), dont souffrent à ce jour, 109 889 patients en France.
« Ce mécanisme d’action a déjà prouvé son efficacité dans les maladies inflammatoires chroniques telles que les maladies rhumatologiques et les maladies dermatologiques, note le Pr Laurent Peyrin-Biroulet, gastro-entérologue et hépatologue au CHRU de Nancy, dans le dossier de presse. Jusqu’à présent, nous disposions de 3 alternatives : les anti TNF alpha, les antiintégrines et les anti-JAK et c’est maintenant la première fois que nous pourrons utiliser un médicament agissant sur la voie de l’interleukine-23 pour le traitement de la RCH, alors que cette molécule est déjà disponible pour la maladie de Crohn depuis plusieurs années » précise-t-il.
UNIFI-I et UNIFI-M
L’efficacité et la tolérance de l’ustekinumab dans cette nouvelle indication ont été évaluées dans le cadre du programme pivotal de phase III UNIFI mené chez des patients ayant présenté une réponse inadéquate ou une intolérance aux traitements conventionnels (corticoïdes, immunomodulateurs) ou aux agents biologiques. La décision d’extension d’indication repose sur une étude d’induction (UNIFI-I) de huit semaines, suivie d’une étude d’entretien (UNIFI-M) de 44 semaines.
L’étude a inclus 961 patients et a été menée sur une durée de huit semaines durant laquelle les patients ont reçu une dose unique d’ustekinumab (dose recommandée d’environ 6 mg/kg ou dose fixe de 130 mg d’ustekinumab, qui n’est pas la dose retenue par l’AMM) ou de placebo par voie intraveineuse. 526 patients en réponse clinique à l’ustekinumab à l’issue de l’étude d’induction pouvaient être inclus dans l’étude d’entretien UNIFI-M où ils ont été randomisés pour recevoir soit 90 mg d’ustekinumab par voie sous-cutanée toutes les huit semaines, soit 90 mg d’ustekinumab par voie sous-cutanée toutes les douze semaines, soit un placebo pendant 44 semaines. Le critère d’évaluation principal de l’étude d’induction était la rémission clinique à la semaine 8 et celui de l’étude d’entretien était la rémission clinique à la semaine 44 chez les patients répondeurs à une perfusion IV unique d’ustekinumab lors de la phase d’induction[2].
Les études UNIFI-I et UNIFI-M ont démontré une efficacité clinique significative à 8 semaines et à 44 semaines versus placebo dans le traitement de la RCH active modérée à sévère, chez des patients adultes présentant une réponse insuffisante, une perte de réponse ou une intolérance à un traitement conventionnel ou à un agent biologique ou qui présentent une contre-indication médicale à ces traitements [2]. Environ 95% des patients en rémission étaient en rémission sans corticoïde à la semaine 44 [2].
Outre un maintien en général de l’efficacité du traitement au bout de 92 semaines, les données à deux ans démontrent aussi qu’environ >95% des patients en rémission symptomatique à S92 sont en rémission sans corticoïde[3].
Un profil de tolérance connu
Les données des études UNIFI-I et UNIFI-M mettent en évidence un profil de tolérance similaire par rapport au profil de tolérance déjà connu de l’ustekinumab qui est maintenant commercialisé depuis dix ans.
Les effets indésirables les plus fréquents (>5%) dans les phases contrôlées des études cliniques conduites avec l’ustekinumab chez les patients adultes atteints de psoriasis, de rhumatisme psoriasique, de la maladie de Crohn et de rectocolite hémorragique étaient des rhinopharyngites et des céphalées. La plupart ont été considérés comme étant légers et n’ont pas nécessité d’interruption du traitement étudié. Les effets indésirables les plus graves rapportés avec Stelara® sont des réactions d’hypersensibilité graves incluant l’anaphylaxie.
Stelara ® en pratique
Stelara® est indiqué dans le traitement de la rectocolite hémorragique active modérée à sévère chez les patients adultes en cas d’échec (réponse insuffisante, perte de réponse, intolérance ou contre-indication) des traitements conventionnels (5-aminosalicylés, corticoïdes et immunosuppresseurs) et d’au moins un médicament biologique parmi les anti- TNFα et le vedolizumab.
Dans la pratique, le traitement est initié par une dose unique en perfusion intraveineuse déterminée en fonction du poids corporel. La première dose sous-cutanée doit ensuite être administrée à la semaine 8 après la dose intraveineuse puis toutes les 12 semaines par voie sous-cutanée 16. Les patients recevant une administration toutes les 12 semaines et qui présentent un échappement après une réponse initiale peuvent bénéficier d’une augmentation de la fréquence d’administration à toutes les 8 semaines. Après une formation appropriée à la technique d’injection sous-cutanée, les patients peuvent s’injecter Stelara® si leur médecin l’estime approprié.
Actualités Medscape © 2021 WebMD, LLC
Citer cet article: Rectocolite hémorragique (RCH): mise à disposition de Stelara®, 1er inhibiteur des interleukines 12 et 23 – Medscape – 12 févr 2021.
La exposición prenatal a #terapia antirretroviral puede contribuir a los cambios cardiacos en los bebés

NUEVA YORK, USA. Los bebés no infectados con virus de inmunodeficiencia humana expuestos a la terapia antirretroviral antes del nacimiento pueden tener cambios cardiovasculares “relevantes”, informan médicos en España.[1]
“Se observó deterioro cardiaco subclínico junto con presión arterial más alta y grosor de la íntima media carotídea más grueso en bebés expuestos al virus de inmunodeficiencia humana a los seis meses de edad. La mitad de ellos presentaba hipertensión”, informaron la Dra. Marta López Carbonell y sus colaboradores, de la Universidad de Barcelona, en Barcelona, España.
“Nuestros hallazgos respaldan posible aumento del riesgo cardiovascular en bebés no infectados por el virus de inmunodeficiencia humana que estuvieron expuestos en el útero a terapia antirretroviral”, escribieron en Clinical Infectious Diseases.
Los investigadores dieron seguimiento a 34 bebés no infectados expuestos al virus de inmunodeficiencia humana y a 53 bebés no expuestos hasta los 6 meses de edad. Los esquemas de terapia antirretroviral durante el embarazo incluyeron dos inhibidores nucleosídicos de la transcriptasa inversa (abacavir más lamivudina: 32%; emtricitabina más tenofovir: 41%, y zidovudina más lamivudina: 21%).
A la edad de 6 meses los lactantes no infectados expuestos al virus de inmunodeficiencia humana tenían paredes miocárdicas más gruesas (grosor medio de la pared septal: 5,02 frente a 3,98 mm; p < 0,001) y disfunción sistólica relativa con disminución del desplazamiento del anillo mitral (8,57 frente a 10,34 mm; p = 0,002 ) y disminución de tricúspide S’ (9,71 frente a 11,54 cm/s; p = 0,003) junto con disfunción diastólica relativa indicada por un tiempo prolongado de relajación isovolumétrica izquierda (58,57 frente a 47,94 ms; p < 0,001).
La evaluación vascular reveló presiones arteriales sistólicas (102 frente a 80 mm Hg; p < 0,001) y diastólicas (64 frente a 55 mm Hg; p = 0,045) significativamente más altas. La mitad de los niños expuestos al virus de inmunodeficiencia humana cumplió los criterios de hipertensión, en comparación con 3,77% del grupo no expuesto (p < 0,001).
Los niños expuestos al virus de inmunodeficiencia humana también tenían grosor de la íntima media carotídea medio más grueso (0,62 frente a 0,51 µm; p = 0,015).
“Estos cambios podrían permitirnos distinguirlos como población en riesgo incluso desde la vida fetal, estableciendo seguimiento estricto y más prolongado”, indicaron los autores.https://8726cd39b10dfee9ce799a8c59060cc7.safeframe.googlesyndication.com/safeframe/1-0-37/html/container.html
“Curiosamente, nuestro estudio muestra por primera vez que la hipertensión infantil podría predecirse a partir de la vida fetal mediante la evaluación de los esquemas maternos de terapia antirretroviral que contienen zidovudina o midiendo el espesor de la pared del tabique fetal mediante ecocardiografía fetal”, añadieron.
Los investigadores agregaron que sus hallazgos también “respaldan la tendencia actual de considerar los esquemas de terapia antirretroviral que contienen zidovudina durante el embarazo como alternativa, debido a la dosificación compleja y la asociación con tasas más altas de efectos adversos leves a moderados”.
Por lo tanto, “evitar los esquemas de terapia antirretroviral que contienen zidovudina durante el embarazo, promover hábitos de estilo de vida saludable y evitar otros riesgos cardiovasculares desde la niñez, podrían potencialmente prevenir eventos cardiovasculares más adelante en la vida”.
El estudio no tuvo financiamiento comercial. Los autores han declarado no tener ningún conflicto de interés económico pertinente. La Dra. López no respondió a una solicitud de comentarios al cierre de la edición.
Traducido y adaptado por el equipo de Medscape en español.
Reuters Health Information © 2021
Citar este artículo: La exposición prenatal a terapia antirretroviral puede contribuir a los cambios cardiacos en los bebés – Medscape – 9 de feb de 2021.
Anticuerpos maternos anti-SARS-CoV-2 cruzan la placenta y se detectan en neonatos

Dra. Naima Joseph
“Creo que el hallazgo más llamativo es que notamos alta respuesta neutralizante a la infección natural incluso en las infecciones asintomáticas, pero naturalmente se observó en mayor grado en personas con infección sintomática”, comentó a Medscape Noticias Médicas la Dra. Naima Joseph, maestra en salud pública de la Emory University School of Medicine, en Atlanta, Estados Unidos.
“Nuestros datos demuestran la capacidad materna para crear respuesta inmunitaria apropiada y robusta”, y la inmunidad protectora materna duró un mínimo de 28 días después de la infección, indicó la Dra. Joseph. “Además observamos títulos en sangre del cordón neonatal más elevados en madres con títulos más altos, lo cual indica una relación, pero necesitamos comprender mejor cómo ocurre la transferencia transplacentaria y establecer correlatos de protección neonatal para ver si la inmunidad materna puede también beneficiar a los recién nacidos, y de qué manera”.
Los investigadores analizaron de forma prospectiva la cantidad de inmunoglobulina G e inmunoglobulina M en muestras de sangre materna y de cordón obtenidas durante el parto de mujeres que resultaron positivas para COVID-19 en algún momento durante la gestación. Utilizaron enzimoinmunoanálisis de adsorción de anticuerpos para el dominio de unión a receptor de proteína en espiga del SARS-CoV-2.
Los 32 pares de madres-lactantes en el estudio fueron predominantemente de raza negra no hispanoamericanas (72%) e hispanoamericanas (25%) y 84% estaba afiliado a Medicaid como su pagador. Mayor proporción de las madres (72%) tenía por lo menos un trastorno concomitante, más frecuentemente obesidad, hipertensión o asma, o enfermedad pulmonar. Poco más de la mitad de las mujeres (53%) tuvo síntomas mientras cursaba con la infección, y 88% enfermó de COVID-19 durante el tercer trimestre. El tiempo promedio desde la infección hasta el parto fue de 28 días.
Todas las madres tenían anticuerpos de inmunoglobulina G, 94% tenía anticuerpos de inmunoglobulina G y 94%tenían anticuerpos neutralizantes contra el SARS-CoV-2. De las muestras de sangre de cordón, 91% tenía anticuerpos de inmunoglobulina G, 9% anticuerpos de inmunoglobulina M y 25% anticuerpos neutralizantes.
“Es tranquilizante que hasta ahora la respuesta fisiológica es exactamente la que esperábamos”, comentó a Medscape Noticias Médicas la Dra. Judette Louis, maestra en salud pública, profesora asociada de obstetricia y ginecología y presidenta del departamento de ginecología de la University of South Florida, en Tampa, Estados Unidos. “Es lo que esperaríamos, pero siempre es útil contar con más datos que respalden esto. Por lo demás, se está extrapolando lo que se sabe de otros trastornos”, destacó la Dra. Louis, quien moderó la sesión de resúmenes orales.
La infección sintomática se asoció con títulos de inmunoglobulina G más elevados de manera estadísticamente significativa que la infección asintomática (p = 0,03), pero no se observó correlación para inmunoglobulina M o anticuerpos neutralizantes. Además, aunque las madres que dieron a luz más de 28 días después de la infección tuvieron títulos de inmunoglobulina G más elevados (p = 0,05), no se observaron diferencias en la respuesta de inmunoglobulina M o neutralizante.
Los títulos en sangre de cordón de los lactantes fueron más bajos de manera estadísticamente significativa que sus muestras maternas correspondientes, sin importar los síntomas o la latencia desde la infección hasta el parto (p < 0,001), informó la Dra. Joseph.
“Se ha demostrado que la eficiencia de transferencia transplacentaria de otros patógenos se correlaciona con la inmunidad neonatal cuando el cociente sangre de cordón/materna es superior a 1”, indicó la Dra. Joseph en su presentación. Sus datos demostraron “eficiencia subóptima” con un índice de 0,81.
El tamaño pequeño de la muestra y la falta de un grupo de control fueron debilidades del estudio, pero una fortaleza importante fue disponer de una población con riesgo desproporcionadamente más alto para la infección y la morbilidad grave que la población general.
Implicaciones para la vacunación materna contra la COVID-19
Aunque todavía no se dispone de los datos, la Dra. Joseph señaló que han ampliado su protocolo para incluir mujeres embarazadas vacunadas.
“La clave para desarrollar una vacuna eficaz para mujeres embarazadas en realidad es caracterizar la inmunidad adaptativa durante la gestación. Creo que estos hallazgos aportan más información para el desarrollo de la vacuna al demostrar que la inmunidad materna es robusta”, añadió la especialista.
La Organización Mundial de la Salud recientemente recomendó no administrar vacunas contra COVID-19 a mujeres embarazadas, pero la Society for Maternal-Fetal Medicine y el American College of Obstetricians and Gynecologists después emitieron una declaración adjunta que reafirma que las vacunas contra COVID-19 autorizadas por la Food and Drug Administration (FDA) de Estados Unidos “no deben dejar de administrarse a personas embarazadas que optan por recibir la vacuna”.[2,3]
“Una pregunta que se plantean es si durante el embarazo se va a generar respuesta satisfactoria a la vacuna de la forma en que ocurriría en personas no embarazadas. Si podemos demostrar que así ocurre, esto puede proporcionar información que algunas madres necesitan para tomar sus decisiones”, señaló la Dra. Louis. Datos como los del estudio de la Dra. Joseph también aportan información para las recomendaciones sobre el momento oportuno de la vacunación materna.
“Por ejemplo, la Dra. Joseph demostró que 28 días después de la infección se tenían más anticuerpos, de manera que puede haber un escenario en que afirmemos que esta vacuna puede ser más beneficiosa a la mitad del embarazo para formar esos anticuerpos”, destacó la Dra. Louis.
Está surgiendo un consenso a partir de los datos de anticuerpos maternos
Los hallazgos del estudio de la Dra. Joseph reflejan los comunicados en un estudio publicado el 29 de enero en la versión electrónica de JAMA Pediatrics. En ese estudio, dirigido por el Dr. Dustin D. Flannery, D. O., del Children’s Hospital of Philadelphia, en Filadelfia, Estados Unidos, también se analizaron los niveles maternos y neonatales de anticuerpos de inmunoglobulina G e inmunoglobulina M contra el dominio que se une al receptor de la proteína en espiga del SARS-CoV-2.[4] Asimismo, se observó correlación positiva entre las concentraciones de inmunoglobulina G en sangre del cordón y materna (p < 0,001), pero notablemente, el coeficiente de títulos en sangre del cordón y materna fue mayor de 1, a diferencia de lo observado en el estudio de la Dra. Joseph.
Para su estudio, Flannery y sus colaboradores obtuvieron sueros de sangre materna y de cordón durante el parto de 1.471 pares de madres y lactantes, independientemente del antecedente de COVID-19 durante el embarazo. La edad materna promedio fue de 32 años, y poco más de una cuarta parte de la población (26%) la constituían mujeres de raza negra no hispanoamericanas. Alrededor de la mitad (51%) era de raza caucásica, 12% hispanoamericanas y 7% asiáticas.
Seis de cada 100 mujeres tenían anticuerpos de inmunoglobulina G o inmunoglobulina M en el parto, y 87% de los lactantes nacidos de estas madres tenía inmunoglobulina G medible en su sangre del cordón.
Ningún lactante tenía anticuerpos de inmunoglobulina M. Al igual que en el estudio presentado en el congreso de la Society for Maternal-Fetal Medicine, las infecciones de las madres incluyeron casos asintomáticos, leves, moderados y graves, y el grado de gravedad de los casos no tuvo efecto ostensible en las concentraciones de anticuerpo del lactante. La mayoría de las mujeres que resultaron positivas en las pruebas para COVID-19 (60%) no tenía síntomas.
De las 11 madres que tenían anticuerpos, pero cuyos lactantes no los tenían en la sangre del cordón, cinco solo tuvieron anticuerpos de inmunoglobulina M y seis tuvieron concentraciones significativamente más bajas de inmunoglobulina G que las observadas en las otras madres.
En un comentario sobre el estudio publicado en JAMA Pediatrics, la Dra. Flor Muñoz, del Baylor College of Medicine, en Houston, Estados Unidos, señaló que los hallazgos son motivo para tener optimismo sobre una estrategia de vacunación materna para proteger a los lactantes contra la COVID-19.
“Sin embargo, el periodo de vacunación materna para proteger al lactante, en contraposición a únicamente a la madre, exigiría un intervalo adecuado desde la vacunación hasta el parto (de por lo menos 4 semanas), mientras que la vacunación en una etapa temprana de la gestación e incluso en una etapa tardía del tercer trimestre podría todavía ser protectora para la madre”, afirmó la Dra. Muñoz.
Dado el intervalo de los esquemas de vacunación de dos dosis y el hecho de que la transferencia transplacentaria comienza más o menos en la semana 17 de la gestación, “la vacunación materna a partir de la primera etapa del segundo trimestre de la gestación podría ser óptima para lograr los máximos niveles de anticuerpos en el recién nacido”, escribió la Dra. Muñoz. Sin embargo, persisten interrogantes, por ejemplo, cuán eficaces son los anticuerpos neonatales para proteger contra la COVID-19 y cuánto tiempo duran después del nacimiento.
No se utilizó ninguna financiación externa en el estudio de la Dra. Joseph.
Las doctoras Joseph y Louis han declarado no tener ningún conflicto de interés económico pertinente. El estudio de JAMA Pediatrics fue financiado por el Children’s Hospital of Philadelphia. Un coautor recibió honorarios por consultoría de Sanofi Pasteur, Lumen, Novavax y Merck, no relacionados con el estudio. Muñoz prestó servicios en las juntas de vigilancia de datos y seguridad de Moderna, Pfizer, Virometix y Meissa Vaccines y recientemente ha recibido becas de Novavax Research y Gilead Research.
Medscape Noticias Médicas © 2021 WebMD, LLC
Citar este artículo: Anticuerpos maternos anti-SARS-CoV-2 cruzan la placenta y se detectan en neonatos – Medscape – 4 de feb de
Terapias dirigidas contra cánceres olvidados
La inmunoterapia está ayudando a mejorar la supervivencia de pacientes de tumores, como el de vejiga, para los que no ha habido avances en 30 años

La inmunooncología es el presente y el futuro del abordaje del cáncer. Este tratamiento ha sido capaz de dar respuesta a enfermedades raras que no tenían terapias específicas hace unos años, mejorando incluso el pronóstico de la enfermedad y la calidad de vida, pero también está demostrando ser capaz de alargar la vida de las personas.
Concretamente, uno de los avances que se están consiguiendo, gracias a la investigación constante, es incrementar la supervivencia de los pacientes con cáncer de vejiga, un tumor en el que no ha habido progresos significativos desde hace 30 años.
Para distinguir las células tumorales de las normales, el sistema inmunitario induce la expresión de proteínas como PDL1 en las células no tumorales, que una vez reconocidas por la proteína PD-1 de los linfocitos impiden el ataque sobre ellas, dirigiéndolo directamente contra el tumor. Pero en ocasiones el tumor es capaz de sintetizar también esta molécula PDL1 como mecanismo de “escape tumoral a sistema inmune”. Los nuevos fármacos anti-PD1 y PDL1 lo contrarrestan y reactivan la respuesta contra el tumor.
“Ésta es la base de la mayoría de los avances terapéuticos que se han producido en la inmunoncología en los últimos cinco años en muchos tumores y de forma especialmente importante dentro de los tumores genitourinarios: en el cáncer de riñón y especialmente en cáncer de vejiga”, explica Jose Angel Arranz, presidente del Grupo Español de Oncología Genitourinaria (SOGUG) y oncólogo en el Hospital Gregorio Marañón, y añade que “estos fármacos han demostrado un incremento significativo de la supervivencia de los pacientes en diferentes escenarios del cáncer renal y de vejiga urinaria”.
El cáncer de vejiga es una enfermedad muy relacionada directamente con el hábito tabáquico; en España hay alrededor de 20.000 casos nuevos al año, siendo el cuarto tumor más frecuente en hombres. Al año, a nivel nacional, fallecen entre 4.400 y 5.000 personas por este tipo de cáncer. El tratamiento tradicional es la resección transuretral del tumor o incluso una cistectomía radical (extirpando la vejiga), es decir, cirugía.
A esto se le suma un tratamiento con quimioterapia perioperatoria que puede ser administrada antes o después de la operación. En la actualidad se están llevando a cabo ensayos clínicos en esta situación con fármacos anti-PD-L1 o anti-PD-1, como tratamiento después de extirpar la vejiga, y de hecho ya sabemos que estos fármacos ofrecen aquí un beneficio adicional prolongando el tiempo hasta la progresión de la enfermedad, y es posible que incluso evitándola en algunos pacientes”, afirma Arranz.
Sin embargo, según destaca el oncólogo, los mayores avances se están observando hasta ahora en pacientes con metástasis, independientemente de que ésta aparezca después de la resección quirúrgica o se diagnostique al inicio. “Hay ya por lo menos seis estudios en marcha que están probando la eficacia de añadir fármacos anti-PD-L1 o anti-PD-1 a la quimioterapia. De hecho, recientemente se ha demostrado que la inmunoterapia aporta resultados prometedores, incrementando la supervivencia global de los pacientes”.
La investigación de tratamientos de inmunoterapia avanza rápido en tipos de cánceres con mayor incidencia, como el cáncer de vejiga, el de mama o el de pulmón. La razón es que hay un mayor número de pacientes para realizar ensayos clínicos; sin embargo, en el panorama de las enfermedades raras el progreso es más lento, pero igual de esperanzador. “Los pacientes de muchas de estas enfermedades raras, como el carcinoma de células de Merkel, un tipo de cáncer de piel más agresivo que el melanoma, no tenían más tratamientos una vez que salían del control quirúrgico. Eran quimioterapias muy poco activas que además se suministraban a un grupo de población ya de por sí frágil como son las personas mayores, inmunodeprimidas y trasplantadas. Se solía recurrir a la cirugía porque no contábamos con más opciones, pero gracias a la inmunoterapia estamos valorando si este tipo de cirugía es realmente necesaria”, afirma Pilar López, oncóloga en el Hospital MD Anderson Cancer Center de Madrid.
La doctora destaca que estos nuevos tratamientos no sustituyen un buen diagnóstico inicial y un buen abordaje precoz, es decir, “si hay un paciente con carcinoma de células de Merkel, se debe hacer una cirugía y un marcaje e incluso ganglios centinela. En fases avanzadas, los nuevos fármacos aportan un beneficio que era desconocido hasta la fecha, pero aún no surten efecto en el cien por cien de los pacientes”, comenta López. La prevención en el caso de esta enfermedad, con una incidencia de uno o dos casos por millón, no es sencilla. Hay tumores de Merkel que, en fases precoces, requieren cirugías poco agresivas. Pero, en otros casos, con tumores más avanzados o pacientes metastásicos, la inmunoterapia marca la diferencia.
“Hace cinco años, cuando veíamos a pacientes con metástasis nos enfrentábamos a una situación muy complicada porque no teníamos nada con qué tratarles. Ahora, gracias a la inmunoterapia contamos ya con resultados del 70% de beneficio claro en pacientes. Hemos pasado de tratamientos con grandes toxicidades, como era la quimioterapia, a fármacos mucho menos tóxicos y más activos”, subraya Pilar López. Ambos expertos destacan la importancia de los ensayos clínicos en el avance de los tratamientos de inmunoterapia. “España es un país privilegiado desde el punto de vista de la participación de pacientes. En todos los ensayos clínicos que han demostrado beneficios de supervivencia o de tiempos de la progresión del tumor, ha habido una amplia participación española, siendo en muchos casos el país que más pacientes ha incorporado a estos estudios”, dice Arranz.
El oncólogo también recalca que el paciente nunca está infratratado en un ensayo clínico, lo habitual es ofrecerle el tratamiento que le correspondería en una situación normal junto al tratamiento en investigación. “Por cuestiones éticas y científicas, el paciente nunca pierde”, concluye.
Con la colaboración de la Alianza Merck-Pfizer.
Que produce cambios en el ADN o infertilidad y que no es segura, bulos que circulan sobre las vacunas de la covid
En un webinar organizado por el Consejo de COF, César Nombela y Marian García desmontaron las ideas erróneas sobre este tratamiento y animaron a los sanitarios a combatirlos.

Las vacunas de la Covid-19 provocan cambios en el ADN porque se incluye dentro de la medicina génica; pueden provocar también infertilidad y no es segura porque los plazos para su aprobación han sido muy cortos, cuando se tarta años en desarrollar un tratamiento de estas características.
Estos son algunos bulos que sobrevuelan a las vacunas de la covid, según se puso de manifiesto en un webinar organizado ayer por el Consejo General de COF, y que pueden poner en peligro los objetivos de inmunización que persiguen las instituciones sanitarias, con el fin de alcanzar la tan conocida inmunidad de rebaño.
En el debate, moderado por Carlos Mateos, coordinador de #SaludsinBulos, participaron Marián García García (@boticariagarcia), divulgadora científica y farmacéutica, y César Nombela Cano, catedrático Microbiología de la Universidad Complutense de Madrid, quienes coincidieron en señalar que esta desinformación se combate con la ciencia y con mensajes sencillos y claros que lleguen a la población, que tiene que tener en sus profesionales sanitarios sus principales referentes para no caer en este tipo de engaños.
Nombela explicó que no es cierto que las vacunas que están administrándose frente al coronavirus produzcan cambios en el ADN y lo hizo con una explicación muy sencilla pero clara: “Las vacunas de ácidos nucleicos, en concreto con ARN son una novedad. Los virus, en concreto los coronavirus, su material genético es ácido ribonucleico, que es un mensajero, que cuando se encuentra con los ribosomas de las células es traducido en proteínas; el virus infecta a la célula y su ácido ribonucleico se adueña de la maquinaria de las proteínas y produce proteínas víricas. El ingenio de estas vacunas ha sido introducir en nuestro organismo una pequeña parte del ácido ribonucleico del virus, la que lleva la información para una proteína, que es la proteína S, que le da el aspecto de corona al virus. De esta forma, nuestras propias células quienes sinteticen esa proteína, como el organismo reconoce esa proteína como extraña se produce una reacción inmunitaria, se desarrollan anticuerpos y células de inmunidad. Y la inmunidad que buscamos es la inmunidad robusta, en la que nuestro organismo reacciona contra el patógeno produciendo anticuerpos y activando células que producen inmnoglobulinas que matan a las que están infectadas por el virus. Hablamos de una inmunidad humoral”.
No es terapia génica
Nombela dice que hay quienes han dicho que estas vacunas no hay que llamarlas así sino terapia génica, “con tono malicioso”, reconoce. De ahí que se pueda pensar que hay cambios en el ADN. A lo que responde: “No hay que llamarlo terapia génica porque eso significa la utilización de procedimientos que cambien algún gen en un organismo enfermo y aquí no se cambia ningún gen, solo se introduce ARN mensajero. No hay una razón lógica para pensar que se pueda producir tal modificación”.
No produce infertilidad
Respecto al bulo de que producen infertilidad, también lo niega y aporta una aclaración: “Algunos han dicho que puesto que estamos produciendo un antígeno contra el que reaccionamos puede dar lugar a reacciones autoinmunitarias. Los problemas autoinmunitarios, de alergias y demás, son muy conocidos, son muy complejos, hay muchos y están muy estudiados y otros, quizás, no tanto. Ahora bien, la proteína de este virus que produce nuestro organismo cuando nos vacunamos y frente a la cual reacciona está mucho más presente si el virus nos infecta. Reacciones autoinmunitarias las hay producidas por patógenos eso es innegable, ahora bien, nada ha demostrado que se produzca una reacción que, además, va en contra de la fertilidad de la mujer, como se ha dicho”.
En cuanto a la seguridad y eficacia de estas vacunas, donde los bulos se ceban especialmente puesto que la cuestionan debido a la rapidez con la que se han aprobado las vacunas, el catedrático de la UCM confirma que los países occidentales dependen de las agencias para la aprobación de los fármacos y cuentan con protocolos de aprobación rápida para situaciones especiales. “Se han condensado las pruebas preclínicas y clínicas en menos tiempo y se ha permitido comparar resultados entre vacunados con personas que han recibido placebo”. En su opinión, se cuenta con la ventaja de que hay muchos vacunados ya, con lo cual ya se dispone de muchísimas información y datos para analizar en otras vacunas no se tenía. No se olvida del seguimiento a dos años que se va a hacer de estos tratamientos.
También añade que cualquier medicamento, y las vacunas lo son, se investigan en arreglo a un proceso muy riguroso y con lo que se denomina calidad farmacéutica.
Miedo a los efectos secundarios
Para Nombela es hasta razonable tener miedo a los efectos secundarios a largo plazo, no obstante insiste en que “todos los medicamentos tienen efectos segundarios, no hay una seguridad cien por cien en la vida ni un riesgo cero”.
En cualquier caso ha mencionado que las que se están administrando actualmente pueden presentar efectos secundarios agudos locales en el lugar de la inyección, fiebre, molestias musculares… “lo que está claro es que la cantidad de ARN inoculado en el organismo no influye en los efectos secundarios que se pudean dar”, aclaró.
Otro de los bulos que se pusieron de manifiesto en el webinar es que la vacuna de la gripe puede producir un empeoramiento de la covid-19, algo que también desmintió Marián García, que dijo que nada tenía que ver una cosa con otra. “La suerte es que este año la incidencia de la gripe es mucho menor gracias a la campaña de vacunación de la gripe que esté año está tiene mayores tasas de cobertura y a las medidas interpuestas como el uso de mascarillas, el lavado de manos, la distancia social y la ventilación de los espacios”.
‘Mejor no vacunarse porque el virus muta’
García García alertó a los farmacéuticos de que pueden llegar pacientes que les digan que es mejor no vacunarse porque el virus muta y la vacuna no será efectiva. Ante esta afirmación, Boticaria Garcia (como así es conocida esta experta) aconseja responder que hay que vacunarse de todas formas, ya que, como aclara Nombela, por la propia tecnología que emplean estas nuevas vacunas hay margen de maniobra para hacer nuevas versiones en poco tiempo.
La responsabilidad de los bulos
Marian García señaló que si existen tantas dudas sobre las vacunas es porque se están haciendo las cosas mal a tres niveles: por una parte las autoridades sanitarias, “a las que les falta pedagogía y sus mensajes no llegan a la población y solo llegan a los informativos noticias de políticos que se vacunan cuando no les corresponde”; por otro, los laboratorios, “que tienen que ser mucho más cautos a la hora de emitir sus notas de prensa, pues la población no siempre está preparada para asimilar lo que dicen; y los medios de comunicación, que no siempre transmiten la mejor información, por ejemplo relacionada con los efectos adversos.
Respecto al papel que pueden ejercer los profesionales sanitarios, en concreto el farmacéutico para combatir estos bulos, García García defendió que es necesario que esté muy formado para ejercer esta labor y dirigirse a fuentes fiables de información. En este sentido, mencionó fuentes como la Organización Mundial de la Salud (OMS), el HNS y la guía sobre covid-19 del Carlos III, que se actualiza cada semana.
Para los sanitarios igualmente es muy útil, según esta farmacéutica, la plataforma sin ánimo de lucro, The Conversations, en la que están incluidos más de 120.000 investigadores que comparten artículos de investigación. Este espacio cuenta con el apoyo de Oxford, Cambridge y la Fundación Bill y Melinda Gates.
En cuanto a las redes sociales, propuso seguir a sanitarios españoles de reconocido prestigio como el intensivista pediátrico, Alberto García Salido, y el inmunólogo Alfredo Correl.
Marián García García también destacó la importancia de formar a todo el equipo de la farmacia que sea un interlocutor con el paciente, pues eso “va a generar confianza en los pacientes”.
La farmacéutica igualmente propuso anticiparse a los bulos que los farmacéuticos detecten en internet y con respuestas sencillas y claras, a veces con humor y otras con otro tono más serio pero siempre con rigor y nunca juzgando a nadie por tener determinadas dudas. Precisamente, sobre los antivacunas, en el debate salió que a los indecisos y a aquellas personas que tienen dudas se les mete en el saco de los antivacunas y eso puede provocar que, realmente se decante por este grupo cuando no lo estaban en un principio.
La falta de vitaminas y minerales, un problema para el 50% de la población
Así lo dice una encuesta realizada a 3.400 personas que acudieron a la farmacia dentro de la campaña ‘¿Conoces el estado de tu sistema inmune?’

Entre el 30 y el 50% de la población tiende a presentar escasos niveles de vitaminas y minerales, según los resultados obtenidos con el análisis de más de 3.400 personas que han acudido a la farmacia dentro de la campaña ¿Conoces el estado de tu sistema inmune?.
La iniciativa, en la que participa la Fundación Alimentación Saludable en colaboración con Arkopharma, se basa en conocer la presencia de vitaminas y minerales de la población y aportarles recomendaciones dietéticas para reforzar el sistema inmunológico en caso de que sea necesario.
En concreto, Los resultados proporcionados por la campaña confirmarn carencias en vitaminas como la C y la D y minerales como el zinc.
Andrea Calderón, secretaria científica de la Fundación Alimentación Saludable, recuerda que las vitaminas y minerales “participan en la síntesis de componentes, como las inmunoglobulinas o los linfocitos, así como en las reacciones bioquímicas que realiza nuestro organismo para combatir agentes externos”. Así, “la vitamina C es clave en la síntesis de colágeno, una barrera natural frente a agentes infecciosos, y su deficiencia puede hacernos más susceptibles a infecciones. Por su parte, minerales, como el hierro, el zinc o el selenio, tienen funciones como antioxidantes y antinflamatorios, esenciales para nuestro sistema de defensas”, añade.
Desde la Fundación Alimentación Saludable recuerda que el seguimiento de una dieta equilibrada y saludable “se asocia con unos mejores valores de inmunidad, como anticuerpos, inmunoglubulinas y linfocitos y se va a ver reflejado en una mayor sensación de vitalidad y energía, y en su conjunto, en un menor riesgo de patologías“.
Embarazadas, lactantes, inmunodeprimidos… quién puede vacunarse y quién no de la covid-19
Tras el inicio de la vacunación de covid-19, surgen las dudas sobre si la inmunización es posible en algunos casos concretos.

La esperada vacunación contra la covid-19 empezó hace unas semanas y según han pasado los días, las dudas han ido apareciendo, tanto entre los enfermos como entre los sanitarios. Al margen de la estrategia de inmunización a grupos de riesgo surgen dudas sobre casos concretos a la hora de recibir la vacuna. ¿Y si estoy embarazada? ¿Y si soy inmunodeprimido? ¿Y si soy alérgico?
Para resolver las preguntas de los profesionales y que estos puedan ofrecer a sus pacientes todas las respuestas, varios organismos han publicado documentos con recomendaciones según grupos de riesgo específicos.
El Hospital Reina Sofía de Córdoba, puso en marcha un teléfono para atender las dudas de los profesionales en este proceso y la junta de de Andalucía tiene un resumen de dichas preguntas. Facme, por su parte, también ha elaborado varios documentos son sugerencias elaboradas por el Grupo de Vacunación del Consejo Asesor de la Federación, demás de la información elaborada por el Ministerio de Sanidad.
Embarazo y lactancia
Una de las dudas más recurrentes es sobre la vacunación en embarazadas y mujeres que están dando el pecho.
Las vacunas actuales son de ARN, no contienen virus vivo, por lo que en principio no debería afectar al feto, pero ante la falta de evidencia científica sobre los posibles efectos secundarios se recomienda de forma general no vacunar a las embarazadas y esperar a que acabe la gestación para administrarla. Asímismo, si se tiene pensado quedarse embarazada, será mejor, como medida de precaución, esperar dos semanas después de la administración de la segunda dosis de la vacuna.
Ahora bien, en el caso de embarazadas que están en primera línea de actuación frente al virus, como pueden ser las sanitarias, con un alto riesgo de exposición al SARS-CoV-2, habría que ponderar el riesgo-beneficio y valorar la vacunación de forma individualizada.
Las mujeres en esta situación deben recibir todos los datos disponibles para tomar una decisión informada al respecto.
En cuanto a las mujeres lactantes, el caso concreto de una psiquiatra que está en periodo de lactancia con su bebé ha tenido gran reflejo en la red social Twitter, ya que en un principio se le negó la vacuna por esta condición. https://platform.twitter.com/embed/index.html?dnt=false&embedId=twitter-widget-0&frame=false&hideCard=false&hideThread=false&id=1349098863244828672&lang=es&origin=https%3A%2F%2Fwww.diariomedico.com%2Fmedicina%2Fmedicina-preventiva%2Fembarazadas-lactantes-inmunodeprimidos-quien-puede-vacunarse-y-quien-no-de-la-covid-19.html&siteScreenName=diariomedico&theme=light&widgetsVersion=ed20a2b%3A1601588405575&width=550px
Las muestras de apoyo y los mensajes de mujeres en situación similar se sucedieron en las redes y finalmente, tras firmar un consentimiento informado, fue vacunada.
La vacuna es compatible con la lactancia, ya que, aunque no hay datos sobre los efectos en este cambio, no contiene virus vivo.
Las recomendaciones de los diferentes organismos indican que la vacunación frente a covid-19 se considera segura para la mujer, la lactancia y el bebé-.
Personas inmunodeprimidas
Las personas inmunodeprimidas o en tratamiento inmunosupresor pueden tener un mayor riesgo de padecer covid-19 grave, por lo que se recomienda la vacunación en este grupo de población, a pesar de que no hay datos sobre la seguridad y eficacia de la inmunización. Asímismo, no se recomienda interrumpir o aplazar el inicio de tratamiento inmunosupresor por motivos relacionados con la vacunación.
El tipo de vacunas basadas en ARN que están disponibles son adecuadas para la administración en pacientes inmunodeprimidos, a pesar de que este grupo de pacientes no ha sido incluido en los ensayos clínicos de las vacunas.
En estos casos se recomienda administrar la vacuna en un momento en el que la enfermedad esté estable o no haya grandes complicaciones, en general a mitad del ciclo de tratamiento.
No se recomienda interrumpir el tratamiento inmunosupresor para recibir la vacuna, ya que podría haber un brote de la enfermedad, ni modificar la pauta de administración del tratamiento, aunque, siempre a valoración del especialista, se podría retrasar la administración de la siguiente dosis no más de dos semanas.
Niños y Adolescentes
Las vacunas aprobadas hasta ahora no han sido testadas en menores de 16 años, por lo que no hay información sobre la eficacia y seguridad en menores de esa edad. Además, no se consideran grupo de riesgo, motivo por el cual no se han incluido en las primeras fases de vacunación.
Sin embargo, hay algunos grupos de niños y adolescentes en los que se podría valorar la conveniencia de la vacunación por soportar una mayor carga de enfermedad, como en aquellos con trastornos neurológicos o discapacidad cognitiva (incluido el síndrome de Down) o los que acuden a centros educativos o residen en instituciones con un riesgo de exposición más elevado.
En cualquier caso, los especialistas deberán ofrecer toda la información a los padres o tutores legales para hacer balance del riesgo-beneficio de la vacunación en estos casos. Aún así, estas recomendaciones podrían cambiar en función de la evidencia que muestre la experiencia con las vacunas y las futuras investigaciones de las mismas en niños y adolescentes.
Pacientes con cáncer
Los pacientes con cáncer deben vacunarse. Debido al mayor riesgo de muerte por covid-19, deben priorizarse los pacientes que están en tratamiento para esta enfermedad, especialmente con cáncer de pulmón o hematológico.
Como en el resto de casos, no hay suficiente evidencia sobre los efectos de las vacunas en estos pacientes, pero, al tratarse de una vacuna basada en ARN, sí hay evidencia para avalar su utilización en pacientes en tratamiento inmunosupresor. Tampoco hay datos sobre la interacción de la vacuna con la quimioterarpia, aunque ésta parece otorgar mayor nivel de anticuerpos neutralizandes que la infección natural, por lo que debe recomendarse que los pacientes con quimioterapia se vacunen. Asímismo, no se debe modificar la pauta de quimioterapia por la vacunación.
Aunque no hay evidencia para recomendar la vacunación en un momento concreto durante la quimioterapia, sería razonable administrar la vacuna entre dos ciclos con medicamentos que puedan disminuir el desarrollo de la respuesta inmune.
En cuanto a la radioterapia, la vacuna puede administrarse durante el tratamiento sin que se realice ninguna modificación en la pauta radioterápica.
Alérgicos
En general puede vacunarse cualquier persona alérgica, excepto aquellos que hayan mostrado alergia a alguno de los componentes de la vacuna. Aún así, y como medida de precaución, las personas con historial de alergia deberían mantenerse en observación durante 30 minutos tras la vacunación. En casos de historia de reacciones alérgicas graves, como por ejemplo anafilaxia, habrá que evaluar el riesgo de la vacunación o mantener la observación tras la misma durante 45 minutos. Si existe historia de reacción alérgica grave a alguno de los componenetes de la vacuna o ha mostrado alergia a la primera dosis, no se podrá administrar la vacuna.
Las vacunas disponibles no contiene trazas de huevo, antibióticos, polietilenglicol, ni látex.
Tratamiento anticoagulante
Los pacientes con trastornos de coagulación o en tratamiento anticoagulante se pueden vacunar ya que la vía de administración no supone ninguna contraindicación.
Sin embargo, en pacientes en tratamiento con fármacos antagonistas de la vitamina K deberán tener un INR dentro del rango terapéutico en un control reciente y no suspender el tratamiento antes de la vacuna.
Si el tratamiento es con anticoagulantes de acción directa (ACOD) o heparinas de bajo peso molecular (HBPM) no es necesario suspender el tratamiento previo a la vacuna, pero se debe evitar administrar la vacuna en las horas próximas al pico máximo de concentración de anticoagulante en plasma.
Se recomienda utilizar un aguja fina (no más de 23G) para la vacunación y presionar la zona del pinchazo durante al menos tres minutos.
En el caso de coagulopatías congénitas o trombopatías, el hematólogo dará las instrucciones oportunas antes de la vacunación.
Por último, en pacientes con trombopenia persistente, si el recuento de plaquetas es mayor de 50.000/mm3 no se precisan medidas especiales, pero si es de 30-50.000 plaquetas/mm3, se recomienda comprimir la zona de punción (sin frotar) durante al menos 3 minutos y una aguja de máximo 23G. En caso de que el recuento de plaquetas sea inferior a 30.000/mm3 se recomienda una valoración individualizada previa por el hematólogo. Si se indica una transfusión de plaquetas, se señalará el tiempo máximo entre transfusión y vacunación. Cuando se vacune, se recomienda comprimir la zona de punción durante al menos 3 minutos y pinchar con calibre máximo de la aguja de 23G.
Esclerosis múltiple
Ninguna de las vacunas covid-19 comercializadas hasta ahora en España está compuesta por virus vivos o atenuados por lo que, en principio, no estarían contraindicadas en pacientes con esclerosis múltiple que se administran un tratamiento modificador de la enfermedad (TME) inmunomodulador o inmunosupresor. Sin embargo, al no haberse incluido en los ensayos de las vacunas personas con esta enfermedad no hay evidencias, no se puede recomendar categóricamente la vacunación, sino una serie de sugerencias al respecto.
La decisión de vacunación debe ser tomada de forma conjunta por el paciente y su Neurólogo/a para establecer un adecuado balance riesgo/beneficio de forma individual en cada caso.
Desde la Sociedad Española de Neurología recomiendan, en caso de vacunación, que el neurólogo haga un seguimiento clínico del paciente que reciba la inmunización para comunicar cualquier efecto adverso, especialmente los relacionados con el sistema nervioso.
Pacientes con covid-19
No se conoce la duración de la inmunidad una vez superada la infección, así que la vacunación está indicada en personas que hayan pasado la covid-19.
En el caso de personas con la infección, ya sea sintomática o asintomática, deberán estar totalmente recuperados de la enfermedad y finalizado el periodo de aislamiento para poder vacunarse, al menos cuatro semanas desde inicio de los síntomas.
Celiacos
No hay ninguna consideración específica que contraindique la vacunación para la covid-19 en personas con celiaquía.
Enfermedades autoinmunes
No hay ninguna consideración específica que contraindique la vacunación para la covid-19 en personas con enfermedades autoinmunes.
Diálisis
No hay ninguna consideración específica que contraindique la vacunación para la covid-19 en personas con este tratamiento.
La saga de la Covid-19 : Partie II

Colas TCHÉRAKIAN, service de pneumologie, hôpital Foch, Suresnes ; Centre de compétence des déficits immunitaires ; Centre de référence des éosinophiles (CEREO)
Covid-19 et formes aiguës : comprendre les tests diagnostiques et leur utilisation – Comprendre l’immunité post-Covid
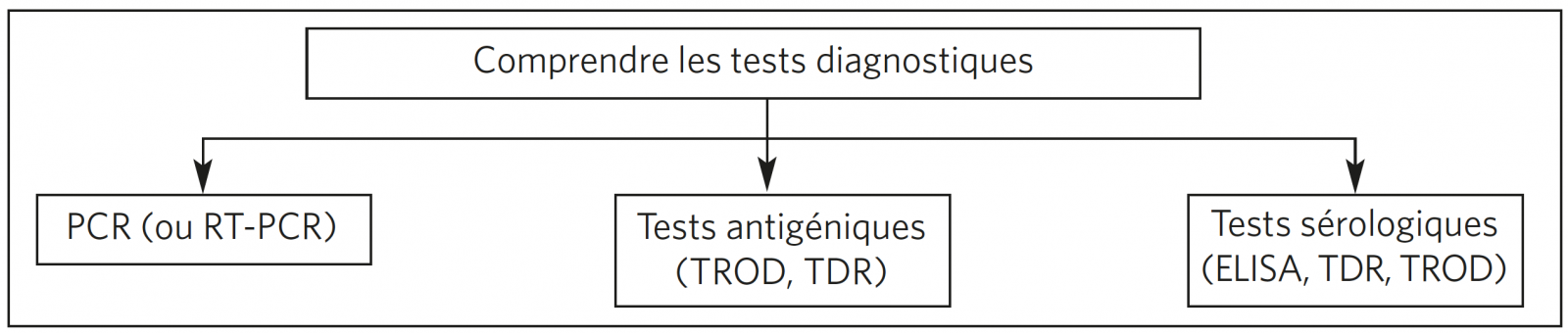
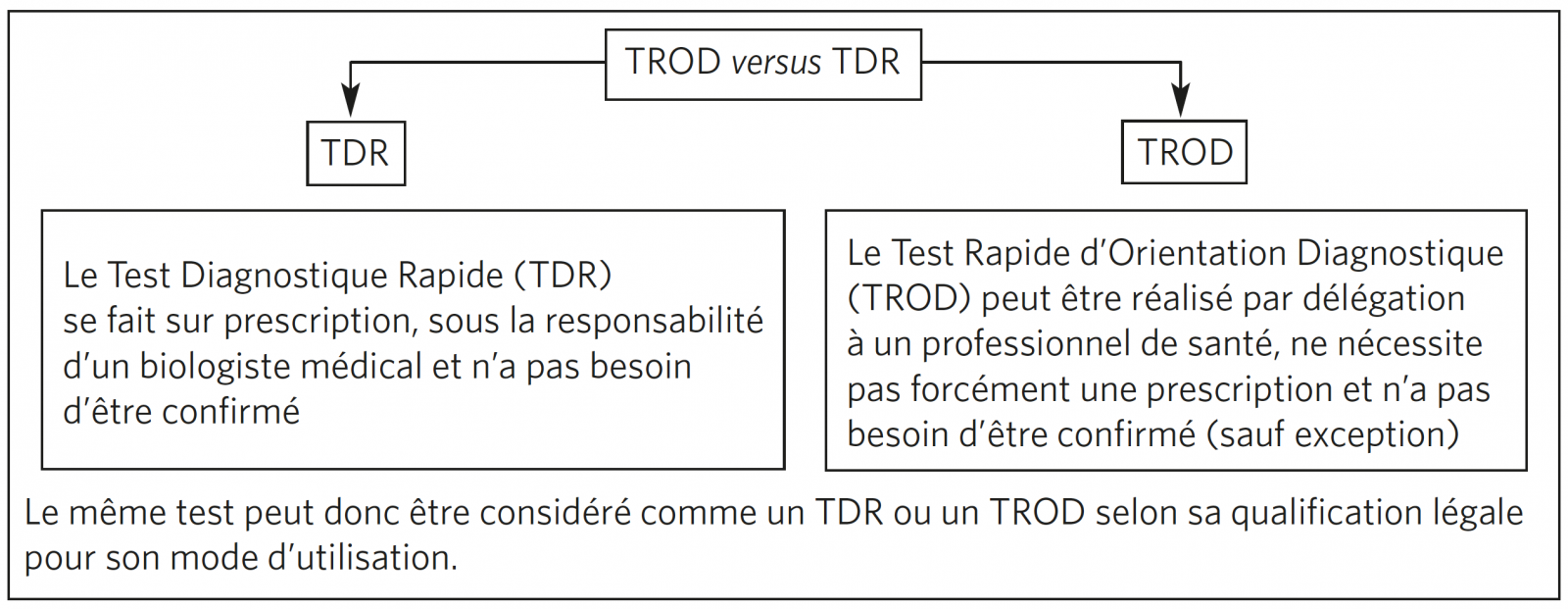
DIFFÉRENTS TESTS DIAGNOSTIQUES : TDR, TROD, PCR OU SÉROLOGIES
Définition et utilisation
À quel moment les prescrire ?

REVUE DES DIFFÉRENTS TESTS
Tests en phase aiguë
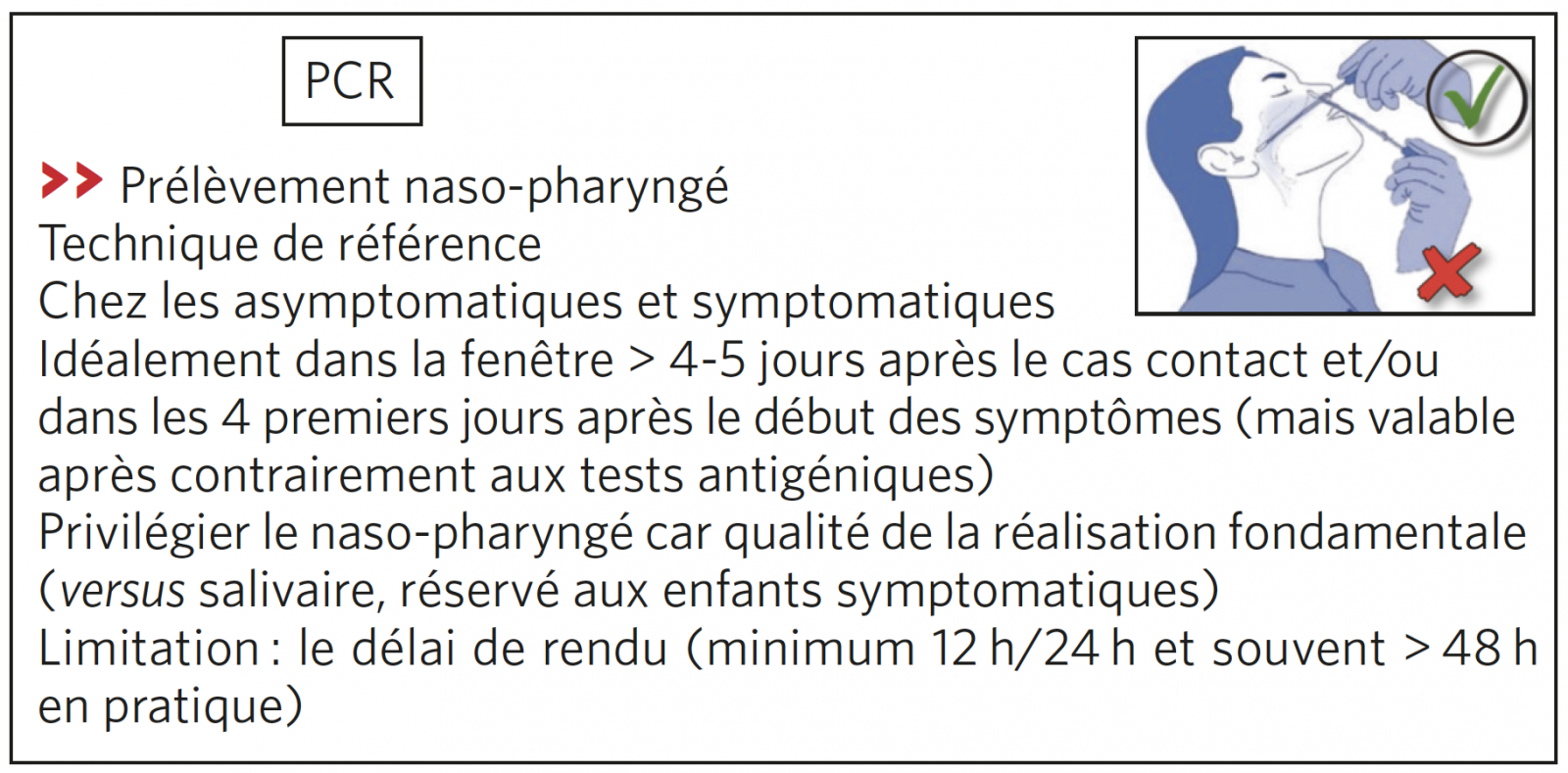
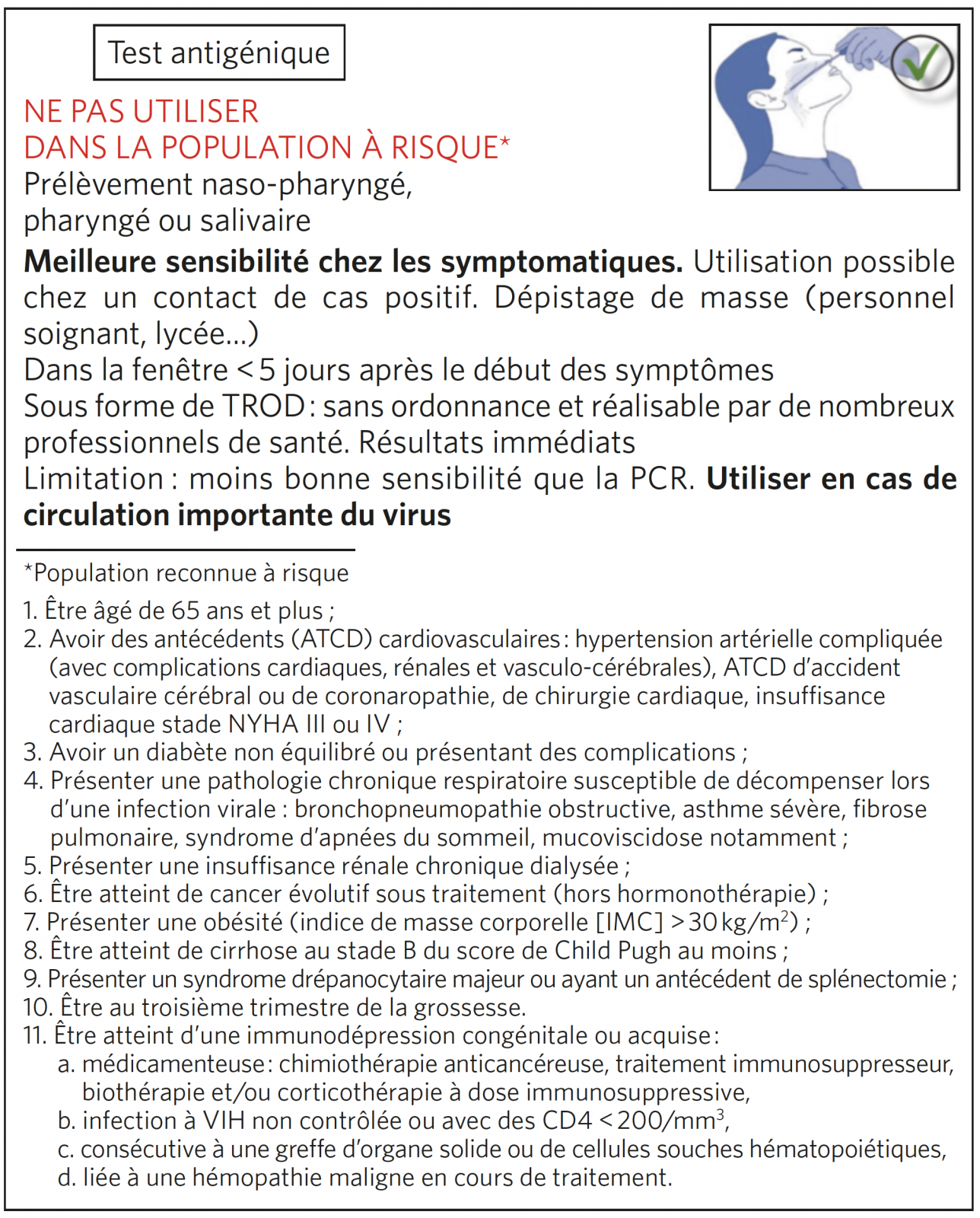
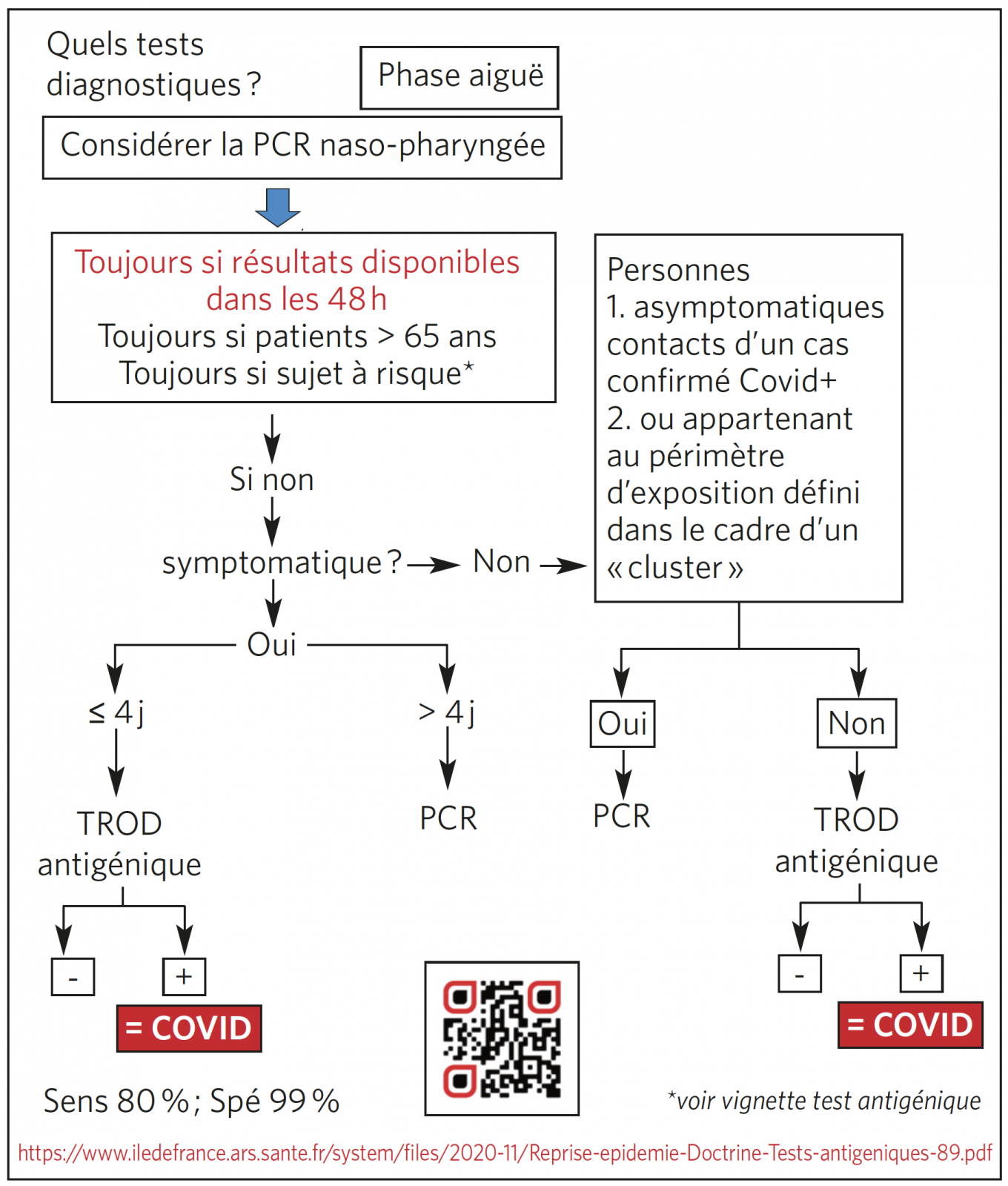
Tests diagnostiques de la phase aiguë : guide d’utilisation
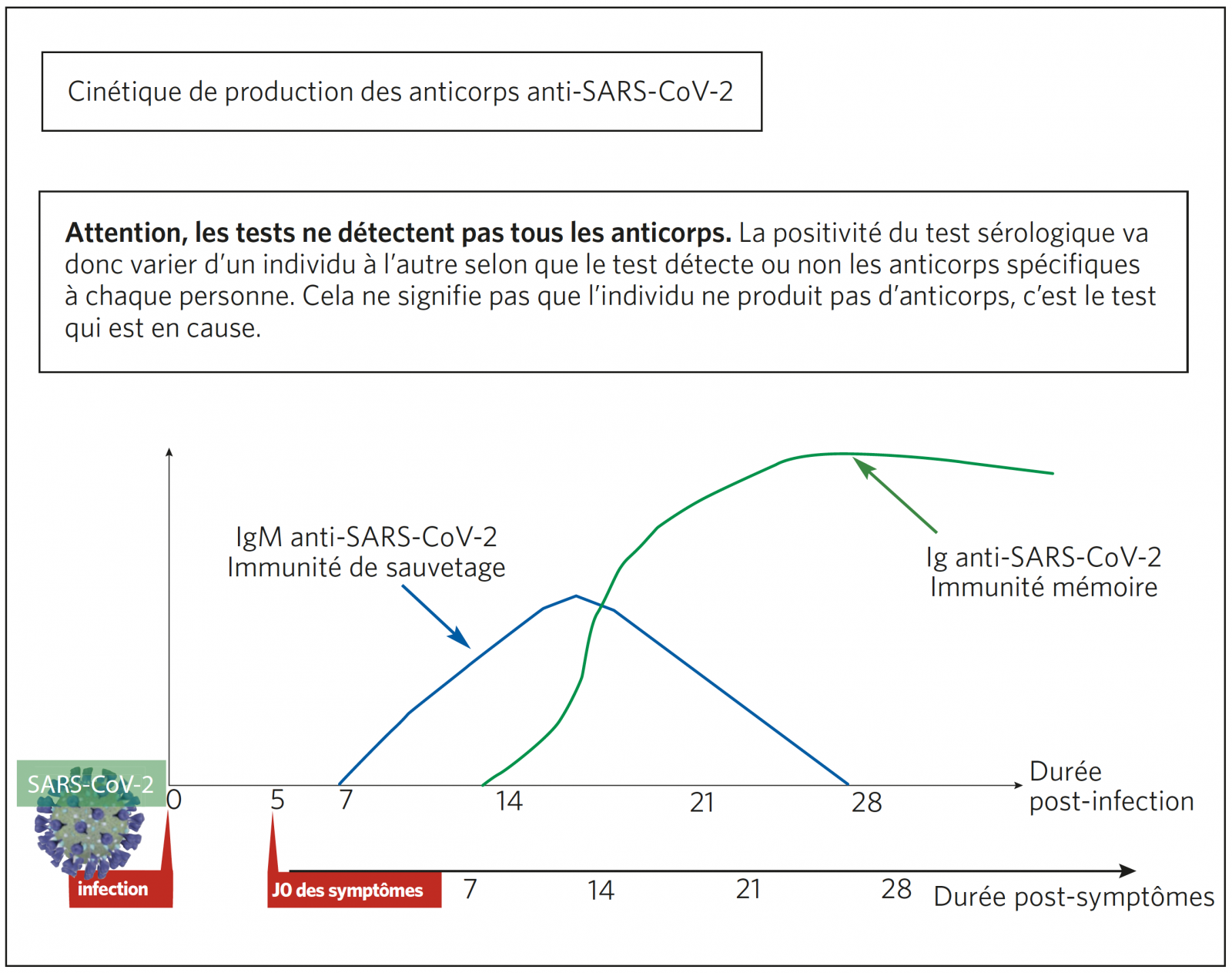
Dynamique des anticorps et interprétation des différentes sérologies (ELISA, TROD sérologiques)
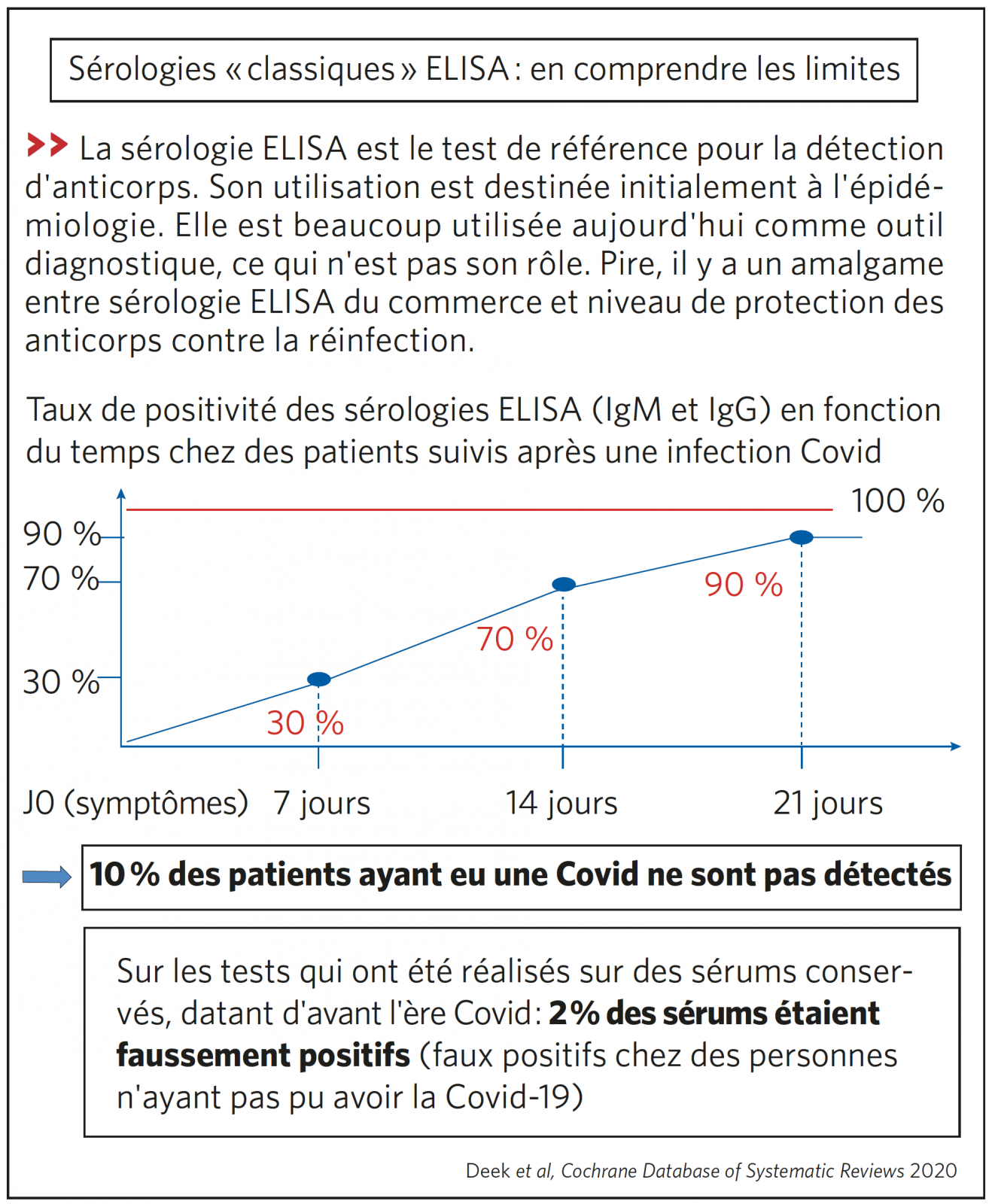
SÉROLOGIE ELISA (TEST DE RÉFÉRENCE)
Sérologie ELISA : exemples de résultats selon la prévalence de la maladie dans la population testée

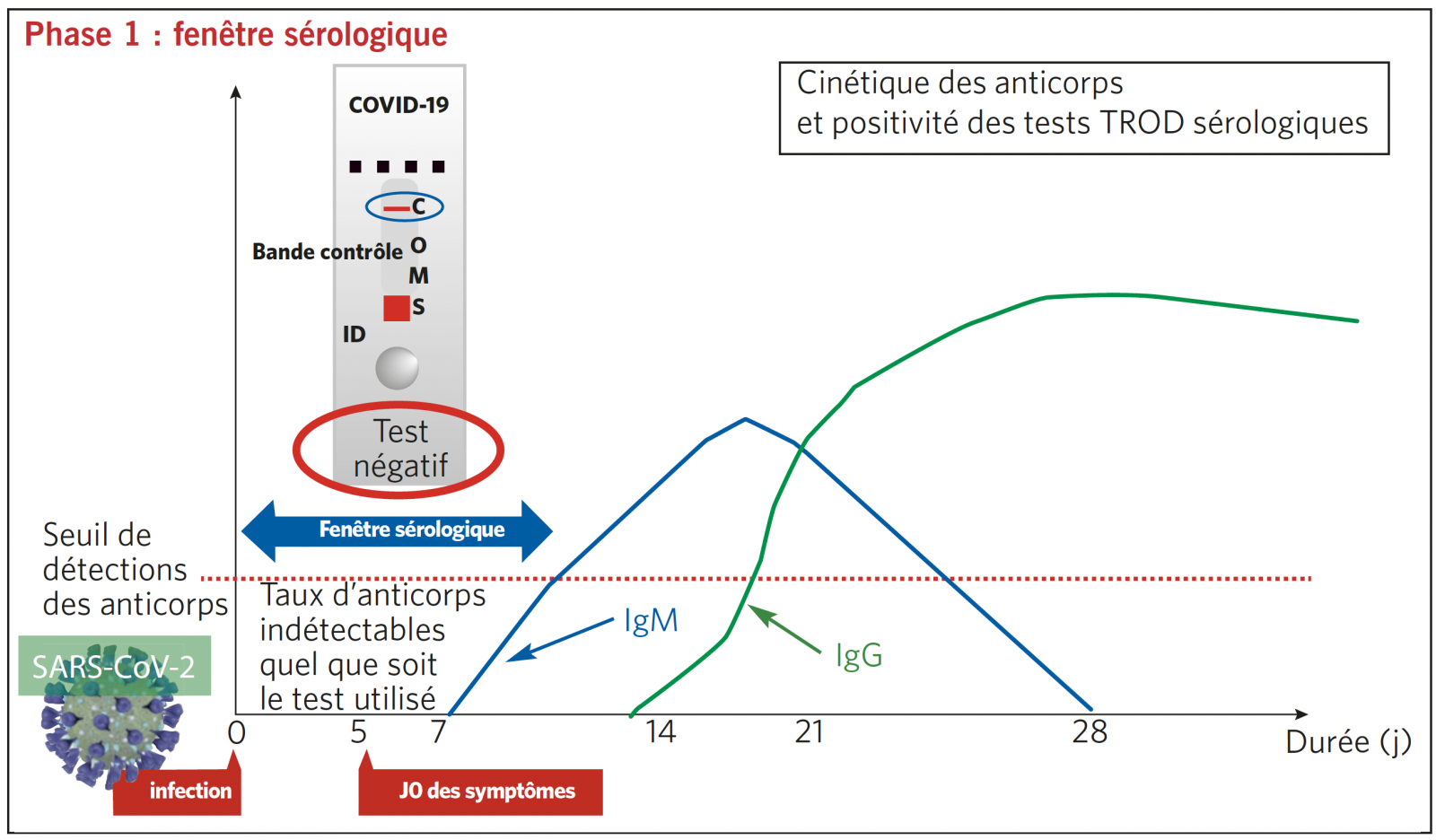
TEST SÉROLOGIQUE TROD : INTERPRÉTATION SELON 4 PHASES SÉROLOGIQUES DE LA MALADIE
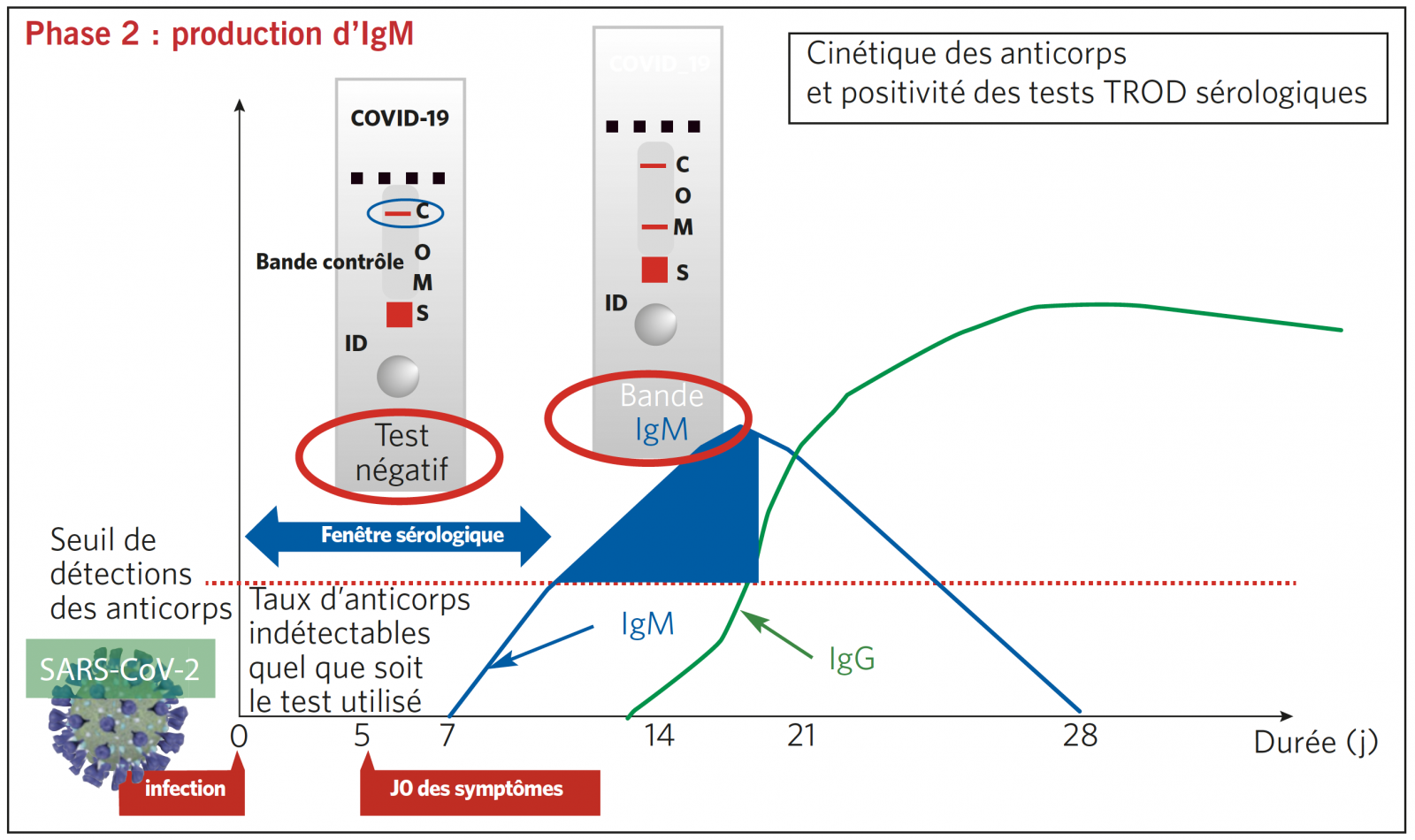
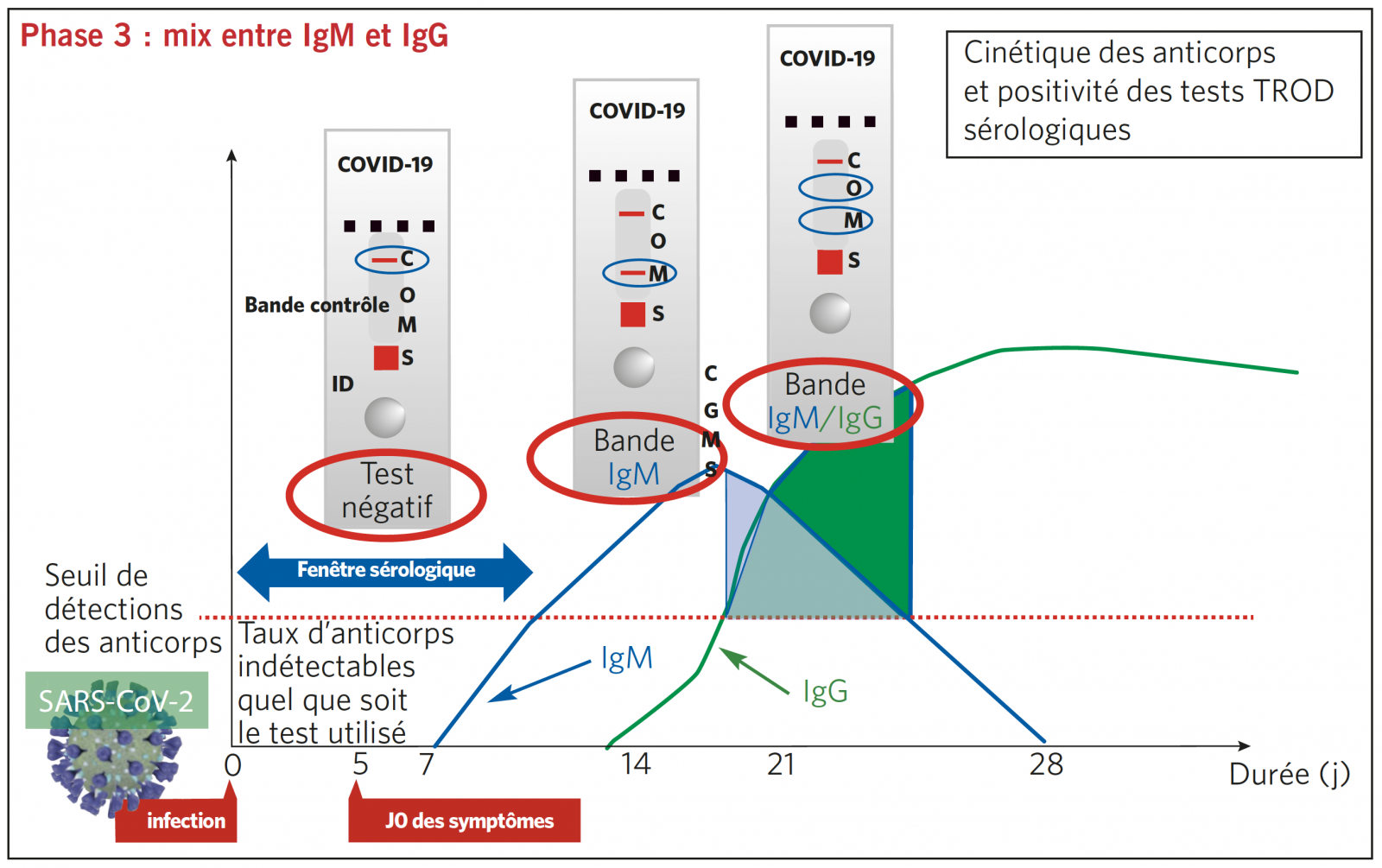
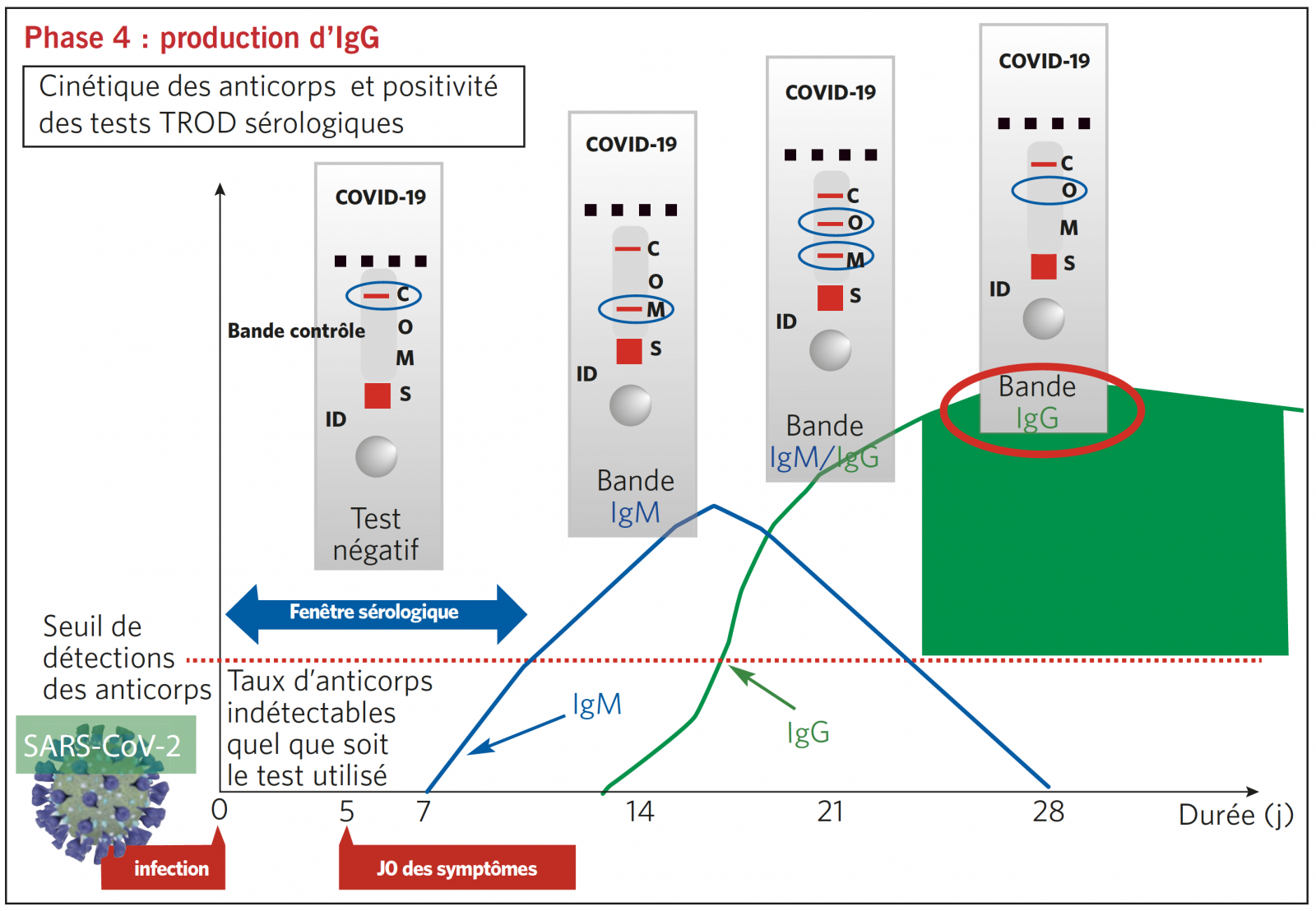
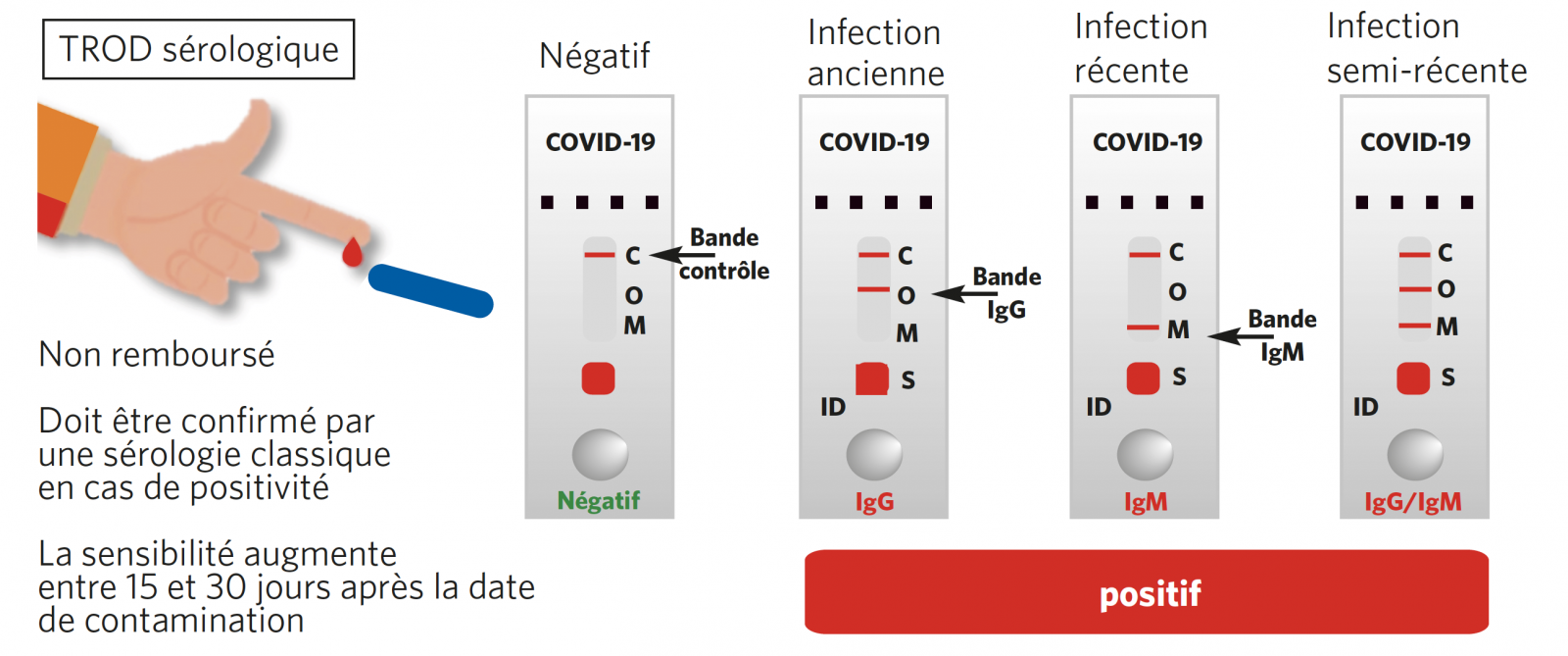
TROD SÉROLOGIQUE EN RÉSUMÉ : RÉPONSE EN < 30 MINUTES
RÉSUMÉ D’UTILISATION DES DIFFÉRENTS TESTS

UN PIED DE NEZ AU VIRUS
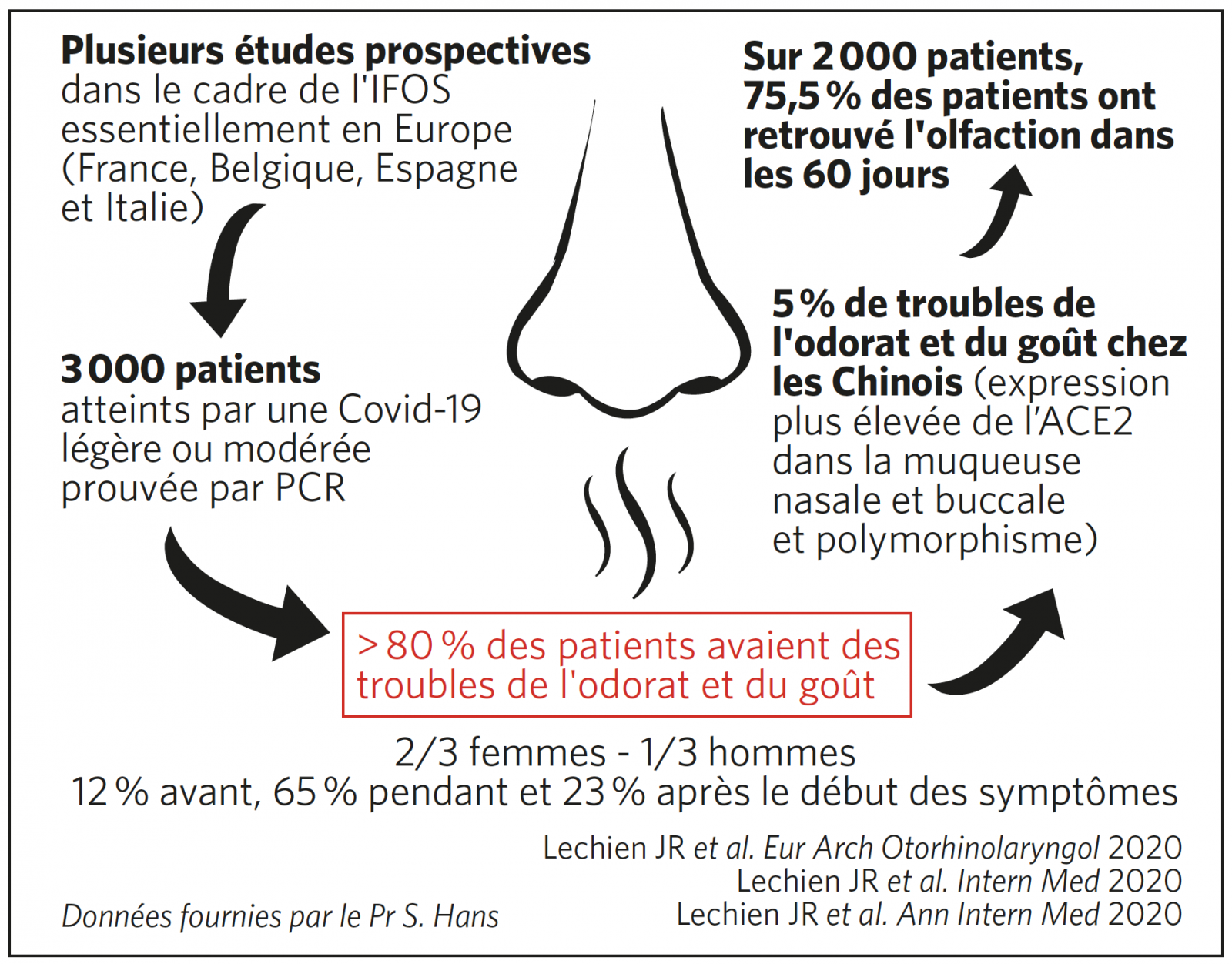
>> L’anosmie, si elle est très handicapante, semble être un facteur de bon pronostic sur l’issue de la maladie. Les IRM réalisées montrent qu’il s’agit d’une atteinte des bulbes olfactifs. Les chiffres ci-dessous montrent combien l’atteinte ORL est fréquente au cours de l’infection par le SARS-CoV-2.
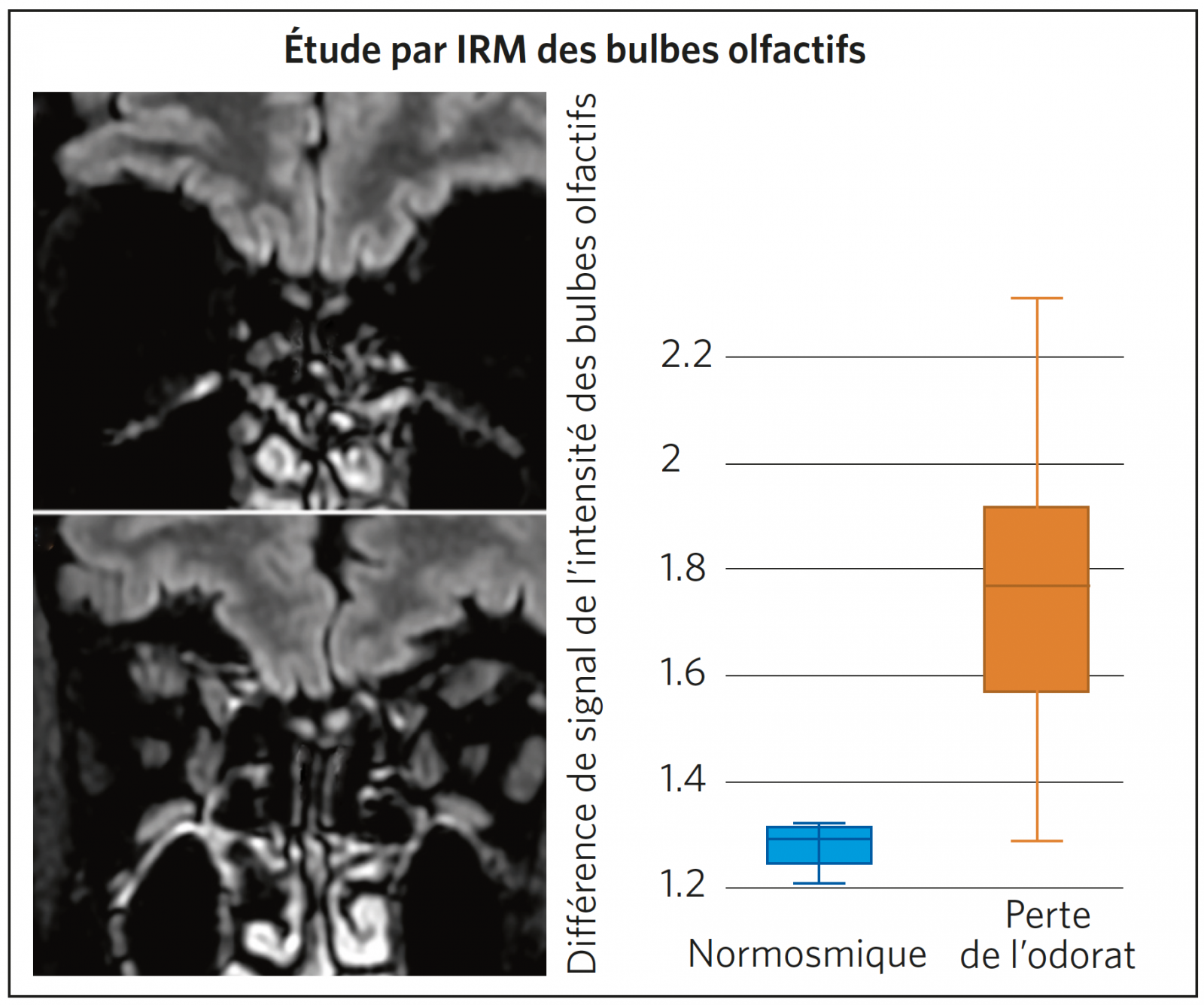
Comparaison des vues coronales T2/FLAIR centrées sur les bulbes olfactifs montrant un signal normal chez un patient normosmique (A) et augmentation d’intensité des bulbes olfactifs chez un patient anosmique (B). Le diagramme en boîte (C) montre que la différence de signal est significative entre les deux types de patients (p < 0,001).
Chetrit A et al. J Infect 2020
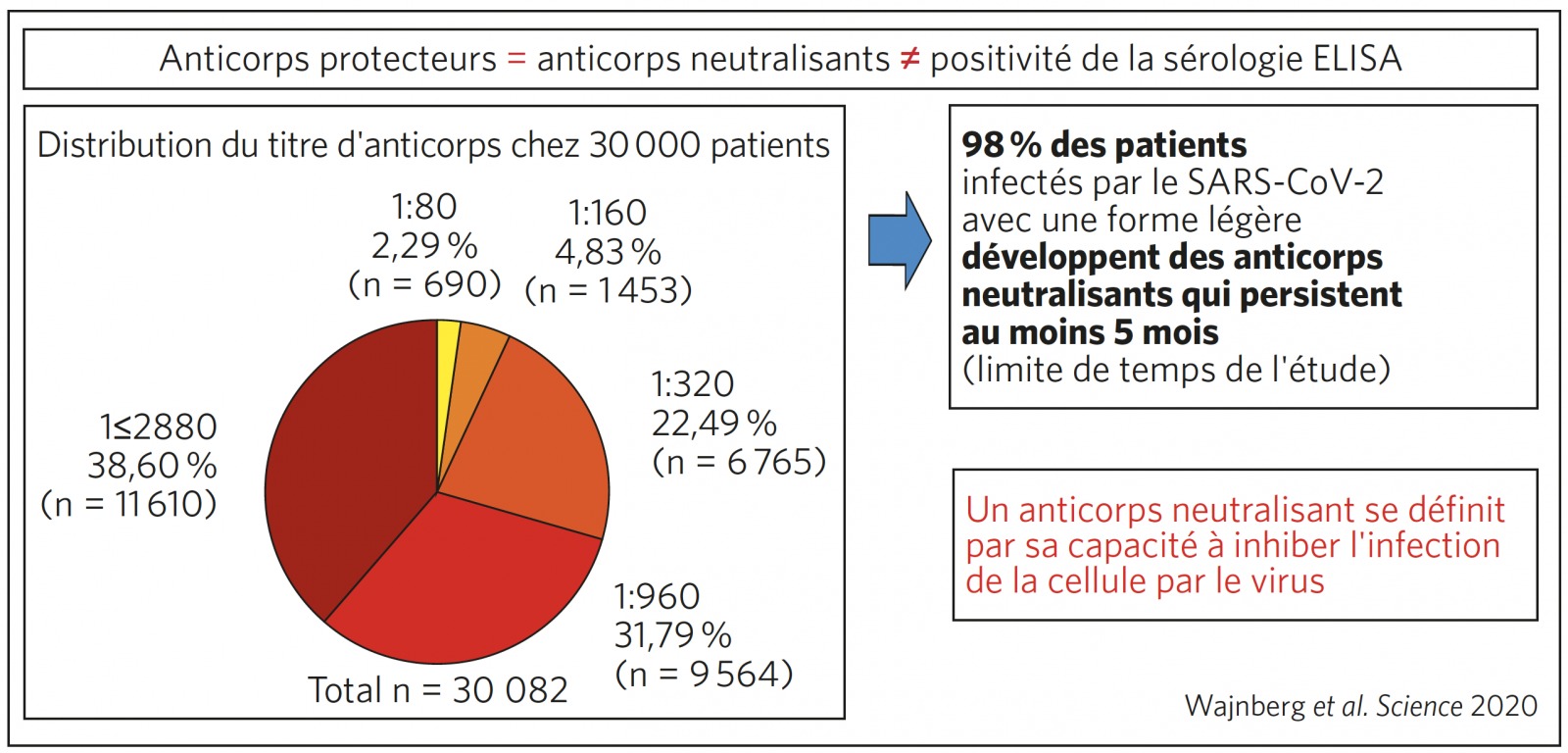
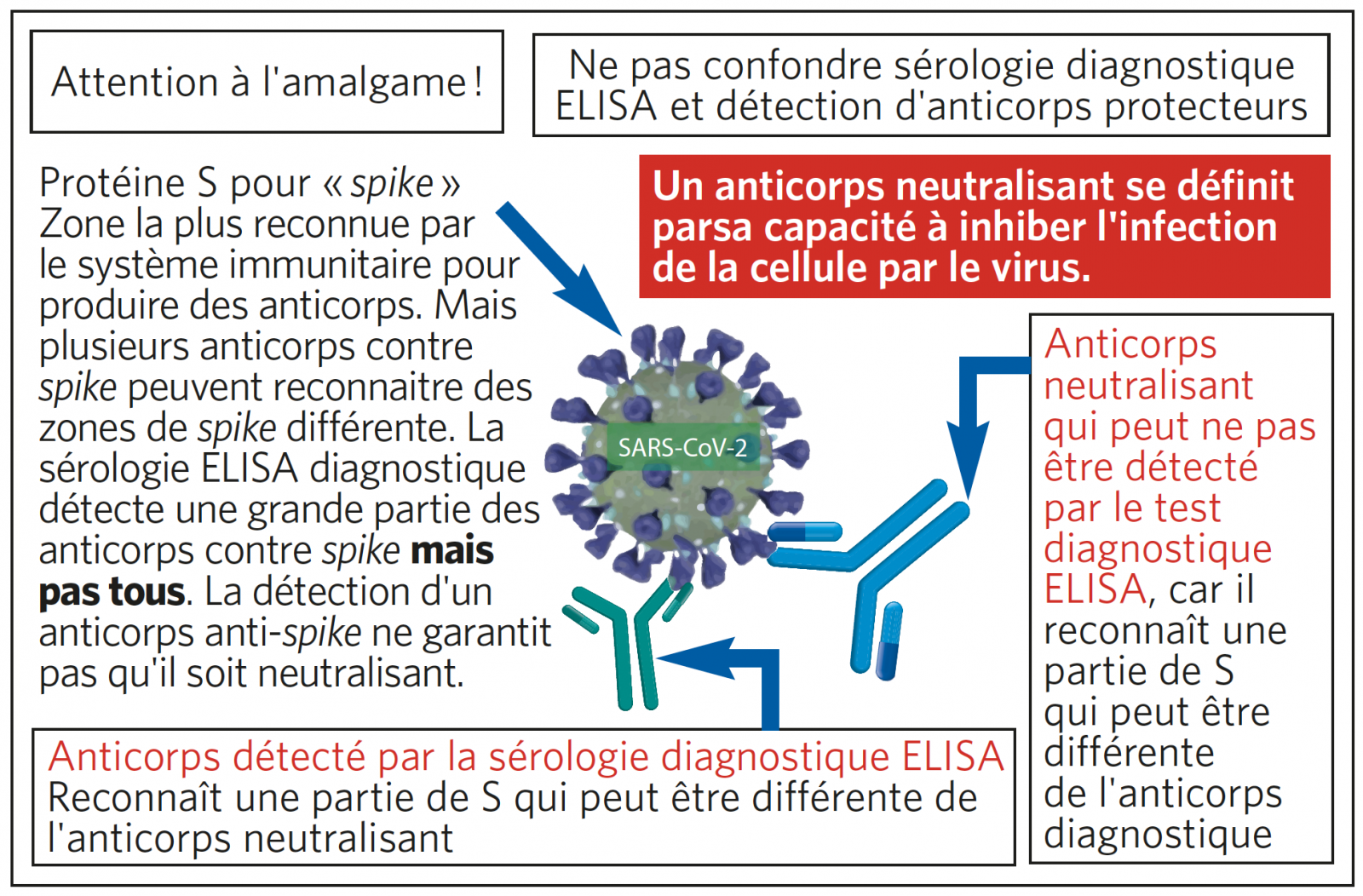
COMPRENDRE L’IMMUNITÉ PROTECTRICE POST-COVID
Il est inutile de faire des sérologies ELISA pour connaître le statut immunitaire d’un patient après une Covid démontrée par PCR. Le résultat de la sérologie ne préjuge pas de l’immunité protectrice contre le SARS-CoV-2.


Publié dans OPA Pratique
Los oncólogos piden vacunar con prioridad a pacientes con tumores avanzados y tratamientos activos
Los pacientes con enfermedad tumoral avanzada y los que están recibiendo terapia activa deberían recibir la vacuna contra el SARS-CoV-2 de forma prioritaria.

“Con cáncer o sin cáncer, las vacunas son seguras. Su mayor o menor eficacia en el tiempo se verá con el tiempo y con los estudios pero, en estos momentos, la única manera de doblegar o solucionar esta situación pandémica es la vacunación masiva. Este es el primer mensaje. En pacientes oncológicos en concreto, no hay ningún grupo que no vaya a obtener beneficio y los riesgos especiales para determinados pacientes -en función de la edad, la patología tumoral, los estadios avanzados y ciertos tratamientos- son elevados, en cuanto a morbimortalidad, por lo que el balance beneficio-riesgo es clarísimo a favor de la vacunación”, indica Álvaro Rodríguez-Lescure, presidente de la Sociedad Española de Oncología Médica (SEOM).
Tras la aprobación de la primera vacuna frente al SARS-CoV-2 por la Agencia Europea del Medicamento (EMA) y la actualización de la Estrategia de vacunación frente el Covid-19 en España realizada por el Ministerio de Sanidad, esta organización ha publicado un documento de posicionamiento y recomendaciones sobre la vacunación en pacientes con cáncer. Esta declaración se ajusta a la que han propuesto otras sociedades internacionales como la Europea de Oncología Médica (ESMO), la Americana para la Investigación del Cáncer (AACR) y en España, la Federación de Asociaciones Científico Médicas (FACME).
Adelantarse a los riesgos
Actualmente, el plan de vacunación en España contempla a los pacientes con cáncer dentro del grupo de personas con condiciones de riesgo: riesgo de morbilidad grave y mortalidad y riesgo de contagio por mayor exposición, debido a la enfermedad y tratamientos oncológicos y visitas frecuentes a entornos asistenciales. “Vacunar es esencial, para todos los colectivos en general y para el oncológico en particular. Pero, de momento, la impresión que impera es que va muy retrasado. Hay que habilitar los medios necesarios para vacunar de forma masiva para restringir morbimortalidades que, desgraciadamente, seguiremos viendo. Hay que proteger a la población cuanto antes”.
Desde el pasado mes de marzo de 2020, se advirtió que los pacientes con cáncer tienen mayor riesgo de enfermedad grave y mortalidad si se infectan con el SARS-CoV-2 y padecer la covid-19 que la población sin cáncer.
Para Rodríguez-Lescure, dentro del paciente oncológico hay que distinguir situaciones diversas y diferentes, pero desde el punto de vista de la Oncología tendrían una mayor prioridad para la vacunación “los pacientes con tumores avanzados o que están recibiendo tratamientos activos. En ellos es fundamental. Los que están en seguimiento o en revisión, con enfermedad controlada o largos supervivientes, por ejemplo, parecen no tener un riesgo tan elevado, en comparación con el de las personas que no ha tenido cáncer”.
No obstante, en el documento elaborado se señala también que aunque los datos para elaborar recomendaciones en pacientes con un diagnóstico anterior de cáncer, los que existen avalan la recomendación de hacerlo en los diagnosticados de cáncer en el último año, ya que se ha observado que también tienen un riesgo más elevado.
Subgrupos más frágiles
Estar recibiendo terapia oncológica activa o tener enfermedad avanzada “es especialmente relevante en los pacientes con cáncer de pulmón y neoplasias hematológicas, independientemente del resto de factores de riesgo, ya que presentan mayores probabilidades de enfermedad grave y mortalidad por covid-19”, señala el presidente de SEOM, quien aclara que también parece que los pacientes con tumores sólidos tienen aumentado el riesgo en el primer año tras el diagnóstico. En cambio, el riesgo desciende pasados los 5 años desde el diagnóstico de cáncer”.
La eficacia de las vacunas aprobadas para la covid-19 de cualquier gravedad se ha establecido en un 95% en la población adulta y de edad avanzada, con un perfil de seguridad aceptable. Sin embargo, según el documento de SEOM, de momento no hay datos suficientes para evaluar las interacciones entre los tratamientos oncológicos con la vacunación contra la covid-19, aunque los ensayos clínicos demuestran que la vacuna puede proporcionar mayores niveles de anticuerpos neutralizantes que la propia infección. Por ello, SEOM señala que debe recomendarse la vacunación en pacientes que reciben tratamientos inmunosupresores.
Sin contraindicaciones
“No hay evidencia de que la inmunoterapia con inhibidores de los puntos de control inmunológico aumente las complicaciones de cualquier vacuna viral. Por tanto, en este caso la vacunación en este grupo no está contraindicada. Se necesita recopilar la información de forma continuada sobre la seguridad y eficacia de la vacuna frente al SARS-CoV-2 en pacientes con cáncer. Así como de sus potenciales interacciones con las terapias antineoplásicas”, indica SEOM.
Para el resto de pacientes con antecedente de cáncer, en seguimiento, esta institución recomienda considerar la edad, estado general y comorbilidades (obesidad, hipertensión, diabetes, patologías respiratorias, cardíacas y renales) o la indicación de vacunación según los grupos establecidos en el Plan de Vacunación del Ministerio de Sanidad.