endocrinologia
Aged 40+ With Diabetes Hit Badly by COVID-19, Should Be Vaccine Priority

People with type 2 diabetes as young as 40 years of age face a disproportionately increased risk of dying from COVID-19 infection, indicates a UK analysis of three large-scale datasets that shines a light on the need to prioritize vaccinations in younger vulnerable patient groups.
The research was published February 8 in the journal Diabetologia.
The majority of European countries have prioritized COVID-19 vaccinations for people with type 2 diabetes, but typically only at age 50 and older. However, the data from the current study suggest that this age limit should be lowered.
“It’s important to remember the risk to middle-aged people with diabetes of dying from COVID-19 is very low in absolute terms compared with the elderly,” said lead researcher Andrew P. McGovern, MD, of Royal Devon & Exeter Hospital, Exeter, United Kingdom, in a press release from his institution.
However, he said that “strategies to define priority groups for vaccination must consider the disproportionate relative risk of COVID-19 mortality in middle-aged people with type 2 diabetes whose COVID-19 risk is already elevated by their age.”
McGovern told Medscape Medical News that the magnitude of the effect of type 2 diabetes on COVID-19 deaths “is really what’s surprising” about these new findings, and “not what you would expect.”
He said it is therefore crucial that people with diabetes are put “into the queue” for the vaccine “in the right place, and obviously in countries where the vaccine rollout will be slower, it is more important.”
Bridget Turner, director of policy campaigns and improvement at Diabetes UK, which funded the study, said the results give “important new insights into how much type 2 diabetes adds to the overall risk of dying from coronavirus at different ages, particularly the additional risk that the condition adds in middle-age.”https://c275ced267b81d32d592c3471da53348.safeframe.googlesyndication.com/safeframe/1-0-37/html/container.html
“The UK has made good progress on prioritizing those who are most vulnerable for vaccination, which includes all adults with diabetes,” she added in the press release, “but we need to continue to work at pace to identify and protect those individuals at higher risk.”
Relationship Between COVID Death and Diabetes Is Complex
The authors note that the relationship between COVID-19-related mortality and type 2 diabetes is not simply an “additive effect of diabetes and age-related risk” but appears to be a “more complex” association, with a “disproportionately higher excess relative mortality risk in younger people with diabetes.”
To investigate this, they examined data from two UK population-based studies that had previously reported age-specific hazard ratios for COVID-19 mortality associated with diabetes:
- OpenSAFELY, which included 17.2 million people, of whom 8.8% had diabetes, and had an overall 90-day mortality rate of 0.06%
- QCOVID, comprising 6 million individuals, of whom 7% had diabetes, and had an overall 97-day mortality rate of 0.07%.
The team also looked at data on type 2 diabetes patients with severe COVID-19 from the COVID-19 Hospitalisation in England Surveillance System (CHESS), which contained 19,256 patients admitted to critical care in England, of whom 18.3% had diabetes.
The 30-day in-hospital mortality rate in this study was 26.4%.
They translated the mortality hazard ratios associated with COVID-19 infection in people with diabetes into a “COVID-age,” which equates to the additional years of “death risk” added to an individual’s chronological age if diabetes is present.https://c275ced267b81d32d592c3471da53348.safeframe.googlesyndication.com/safeframe/1-0-37/html/container.html
Taking the QCOVID dataset as an example, the results showed that the “COVID-age” associated with diabetes for someone aged 40 years was 20.4 years; that would indicate that their “mortality risk [for COVID-19] is similar to that of a 60-year-old person without diabetes.”
The impact of diabetes on the COVID-19 death risk decreased with increasing age, such that a diabetes patient aged 50 years had a COVID-age of 16.4 years. This fell to 12.1 years in someone aged 60, and 8.1 years in someone 70 years of age, which means the latter has the same risk of death from COVID-19 as someone without diabetes who is 78.
Similar results were obtained when the team looked at data from the OpenSAFELY study.
But when they looked at the effect of diabetes on COVID-19 mortality risk in the CHESS dataset, it was less pronounced.
Just Looking at Diabetes Is Oversimplistic, but It’s an Easy Marker for Vaccination
The researchers acknowledge that “considering only age and diabetes status when assessing COVID-19-associated risks…is an oversimplification,” as factors such as body mass index (BMI), diabetes duration, and glycemic control are also known to play a role.
However, they say consideration of these factors is “not practical for population-level vaccine rollout.”
“The time-critical nature of population COVID-19 vaccination necessitates pragmatic group-level prioritization, which is the approach initiated by governments thus far,” the team concludes.
This study was supported by Diabetes UK. Study author John M. Dennis is supported by an Independent Fellowship funded by Research England’s Expanding Excellence in England (E3) fund and by the NIHR Exeter Clinical Research Facility. McGovern is supported by the NIHR Exeter Clinical Research Facility.
Diabetologia. Published online February 8, 2021. Full text
Medscape Medical News © 2021
Cite this: Aged 40+ With Diabetes Hit Badly by COVID-19, Should Be Vaccine Priority – Medscape – Feb 15, 2021.TOP PICKS FOR YOU
SOLOIST-WHF démontre les bénéfices de la sotagliflozine dans l’insuffisance cardiaque aiguë du patient diabétique

Patrice DARMON, Marseille
Les inhibiteurs des co-transporteurs du sodium-glucose de type 2 (iSGLT2) ont largement démontré leurs bénéfices dans la prévention des hospitalisations pour insuffisance cardiaque chez les patients diabétiques de type 2 (DT2) à haut et très haut risque cardiovasculaire et dans le traitement de l’insuffisance cardiaque à fraction d’éjection du ventricule gauche (FEVG) diminuée en présence comme en l’absence de diabète.
La sotagliflozine est un iSGLT2 inhibant également les co-transporteurs du sodium-glucose de type 1 (iSGLT1) au niveau intestinal ; à ce jour, ce double inhibiteur SGLT1/2 n’est autorisé qu’en Europe, comme traitement adjuvant du diabète de type 1 chez les patients en surpoids (IMC ≥ 27 kg/m2). L’objectif de l’étude SOLOIST-WHF était d’évaluer les bénéfices et les risques de la sotagliflozine dans le contexte particulier de l’insuffisance cardiaque aiguë chez des patients DT2. L’essai a dû être stoppé prématurément en raison du désengagement financier du sponsor durant la pandémie de la Covid-19, mais des résultats très positifs ont été présentés au cours du dernier congrès virtuel de l’American Heart Association et publiés simultanément dans le New England of Medicine.
L’étude a inclus 1 222 patients DT2 âgés de moins de 85 ans hospitalisés pour décompensation d’une insuffisance cardiaque avec nécessité d’un recours à des diurétiques en intraveineux et élévation significative des taux de peptides natriurétiques. Les critères d’exclusion étaient les suivants : insuffisance cardiaque terminale ; syndrome coronarien aigu, revascularisation coronarienne ou accident vasculaire cérébral récents ; DFGe < 30 ml/min/1,73 m2 ; instabilité clinique (définie par le besoin de recourir à une oxygénothérapie ou à un traitement inotrope ou vasodilatateur en intraveineux — à l’exception des dérivés nitrés — ou de poursuivre les diurétiques en intraveineux ou par une pression artérielle systolique < 100 mmHg). Les sujets ont été randomisés pour recevoir de la sotagliflozine (200 mg/j, pouvant être augmentée à 400 mg/j en l’absence d’effets secondaires) ou un placebo, soit avant la sortie (48,8 % des cas), soit dans les trois jours suivant la sortie (51,2 %). Les caractéristiques des patients à l’inclusion étaient les suivantes : âge médian 70 ans ; 33,7 % de femmes ; IMC 30,8 kg/m2 ; FEVG 35 % (< 50 % dans 79,1 % des cas) ; NT-proBNP 1799,7 pg/ml ; DFGe 49,7 ml/min/1,73 m2 ; HbA1c 7,1 %. Le critère primaire de jugement, modifié à l’arrêt des inclusions pour augmenter la puissance de l’étude, était un critère composite des décès d’origine cardiovasculaire et du nombre total d’hospitalisations et de visites en urgence pour insuffisance cardiaque. Au terme d’un suivi médian de seulement 9 mois, ce critère était réduit de façon significative sous sotagliflozine (51,0 vs 76,3 événements pour 100 patients-années ; HR 0,67 [IC95% 0,52-0,85], p < 0,001). Ce bénéfice était retrouvé à l’identique dans tous les sous-groupes étudiés (hommes ou femmes, âge < ou ≥ 65 ans, origine géographique des centres, traitement débuté avant ou après la sortie, FEVG < ou ≥ 50 %, DFGe < ou ≥ 60 m/min/1,73 m2). Le bénéfice de la sotagliflozine est également retrouvé sur le critère de jugement initialement prévu (décès cardiovasculaire ou première hospitalisation pour insuffisance cardiaque) avec un HR à 0,71 (IC95% 0,56-0,89). À l’inverse, la réduction observée du risque de décès d’origine cardiovasculaire et de décès de toutes origines n’était pas significative (HR 0,84 [IC95% 0,58-1,22] et HR 0,82 [IC95% 0,59-1,14], respectivement).
Les données sur la sécurité de la sotagliflozine, et plus particulièrement sur les événements liés à la déplétion volémique, étaient très attendus dans ce contexte d’insuffisance cardiaque aiguë, et elles sont rassurantes : pas de différence significative entre sotagliflozine et placebo pour les épisodes d’hypotension (6,0 % vs 4,6 %) et d’insuffisance rénale aiguë (4,1 % vs 4,4 %). Les seuls effets indésirables retrouvés plus souvent sous sotagliflozine étaient les diarrhées (6,1 % vs 3,4 %), les hypoglycémies sévères (1,5 % vs 0,3 %) et les infections génitales (0,8 vs 0,2 %) ; les épisodes d’acidocétose étaient rares et moins fréquents sous sotagliflozine que sous placebo (0,3 % vs 0,7 %).
Au final, en dépit de son interruption prématurée, cet essai démontre que la sotagliflozine a un rapport bénéfices-risques hautement favorable en cas d’insuffisance cardiaque aiguë chez le patient diabétique de type 2, et ce, quelle que soit la FEVG. Il s’agit là d’une nouvelle preuve des bénéfices de l’inhibition de SGLT2 en cas d’insuffisance cardiaque, ici dans la situation très particulière de la période post-décompensation. Il reste à déterminer si l’inhibition de SGLT1 induite par la sotagliflozine apporte un bénéfice spécifique chez ces patients.
Publié par Diabétologie Pratique
Références
Cliquez sur les références et accédez aux Abstracts sur 
Bhatt DL et al., for the SOLOIST-WHF Investigators. Sotagliflozin in patients with diabetes and recent worsening heart failure. N Engl J Med 2020 Nov 16. Rechercher l’abstract
Gestational Diabetes Carries CVD Risk Years Later

Erica P. Gunderson, PhD
Women who’ve had gestational diabetes are 40% more likely to develop coronary artery calcification later in life than those who have never had it, and attaining normal glycemic levels doesn’t diminish their midlife risk for atherosclerotic cardiovascular disease.
“The new finding from this study is that women with gestational diabetes had twice the risk of coronary artery calcium, compared to women who never had gestational diabetes, even though both groups attained normal blood sugar levels many years after pregnancy,” lead author Erica P. Gunderson, PhD, MS, MPH, said in an interview about a community-based prospective cohort study of young adults followed for up to 25 years, which was published in Circulation (2021 Feb 1. doi: 10.1161/CIRCULATIONAHA.120.047320).
Previous studies have reported a higher risk of heart disease in women who had gestational diabetes (GD) and later developed type 2 diabetes, but they didn’t elucidate whether that risk carried over in GD patients whose glycemic levels were normal after pregnancy. In 2018, the American College of Cardiology/American Heart Association Cholesterol Clinical Practice Guidelines specified that a history of GD increases women’s risk for coronary artery calcification (CAC).
This study analyzed data of 1,133 women ages 18-30 enrolled in the Coronary Artery Risk Development in Young Adults (CARDIA) study who had no diabetes in the baseline years of 1985-1986 and had given birth at least once in the ensuing 25 years. They had glucose tolerance testing at baseline and up to five times through the study period, along with evaluation for GD status and coronary artery calcification CAC measurements at least once at years 15, 20 and 25 (2001-2011).
CARDIA enrolled 5,155 young Black and White men and women ages 18-30 from four distinct geographic areas: Birmingham, Ala.; Chicago; Minneapolis; and Oakland, Calif. About 52% of the study population was Black.
Of the women who’d given birth, 139 (12%) had GD. Their average age at follow-up was 47.6 years, and 25% of the GD patients (34) had CAC, compared with 15% (149/994) in the non-GD group.
Gunderson noted that the same relative risk for CAC applied to women who had GD and went on to develop prediabetes or were diagnosed with type 2 diabetes during follow-up.https://659177c6dbc0aa51a616452f311f1d01.safeframe.googlesyndication.com/safeframe/1-0-37/html/container.html
Risks Persist Even in Normoglycemia
In the GD group, the adjusted hazard ratio for having CAC with normoglycemia was 2.3 (95% confidence interval, 1.34-4.09). The researchers also calculated HRs for prediabetes and incident diabetes: 1.5 (95% CI, 1.06-2.24) in no-GD and 2.1 (95% CI, 1.09-4.17) for GD for prediabetes; and 2.2 (95% CI, 1.3-3.62) and 2.02 (95% CI, 0.98-4.19), respectively, for incident diabetes (P = .003).
“This means the risk of heart disease may be increased substantially in women with a history of gestational diabetes and may not diminish even if their blood-sugar levels remain normal for years later,” said Gunderson, an epidemiologist and senior research scientist at the Kaiser Permanente Northern California Division of Research in Oakland.
“The clinical implications of our findings are that women with previous GD may benefit from enhanced traditional CVD [cardiovascular disease] risk factor testing – i.e., for hypertension, dyslipidemia, and hyperinsulinemia,” Gunderson said. “Our findings also suggest that it could be beneficial to incorporate history of GD into risk calculators to improve CVD risk stratification and prevention.”
Strong Findings Argue for More Frequent CVD Screening
These study results may be the strongest data to date on the long-term effects of GD, said Prakash Deedwania, MD, professor of cardiology at the University of California, San Francisco. “It’s the strongest in the sense in that it’s sponsored, involved four different communities in different parts of the United States, enrolled individuals when they were young and followed them, and saw very few patients drop out for such a long-term study.” The study reported follow-up data on 72% of patients at 25 years, a rate Deedwania noted was “excellent.”
“Patients who have had GD should be screened aggressively – for not only diabetes, but other cardiovascular risk factors – early on to minimize the subsequent risk of cardiovascular disease is a very important point of this study,” he added. In the absence of a clinical guideline, Deedwania suggested women with GD might have screening for CV risk factors every 5-7 years depending on their risk profile, but emphasized that parameter isn’t settled.
Future research should focus on the link between GD and CVD risk, Gunderson said. “Research is needed to better characterize the severity of GD in relation to CVD outcomes, and to identify critical pregnancy-related periods to modify cardiometabolic risk.” The latter would include life-course studies across the full pregnancy continuum from preconception to lactation. “Interventions for primary prevention of CVD and the importance of modifiable lifestyle behaviors with the highest relevance to reduce both diabetes and CVD risks during the first year postpartum merit increased research investigation,” she added.https://659177c6dbc0aa51a616452f311f1d01.safeframe.googlesyndication.com/safeframe/1-0-37/html/container.html
Future studies might also explore the role of inflammation in the GD-CVD relationship, Deedwania said. “My hypothesis is, and it’s purely a hypothesis, that perhaps the presence of coronary artery calcification scores score in these individuals who were described as having normal glucose but who could be at risk could very well be related to the beginning of inflammation.”
Gunderson and Deedwania have no financial relationships to disclose. The study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases and the National Heart, Lung, and Blood Institute.
This article originally appeared on MDedge.com, part of the Medscape Professional Network.
Medscape Medical News © 2021 WebMD, LLC
Cite this: Gestational Diabetes Carries CVD Risk Years Later – Medscape – Feb 01, 2021.
Surdosage en #vitamine D : éviter les compléments alimentaires chez l’enfant

France– La supplémentation en vitamine D est recommandée dès les premiers jours de vie et jusqu’à 18 ans, afin de prévenir le rachitisme. Cependant, l’Agence nationale de sécurité du médicament et des produits de santé (ANSM) souhaite alerter sur le risque de surdosage suite à la prise de compléments alimentaires enrichis en vitamine D. Des cas ont été récemment rapportés chez des jeunes enfants, ayant entraîné une hypercalcémie pouvant avoir des conséquences graves, telles qu’une atteinte rénale à type de lithiase / néphrocalcinose[1].
Quels risques avec les compléments alimentaires ?
Le risque de surdosage en vitamine D est supérieur avec les compléments alimentaires qu’avec les médicaments pour plusieurs raisons :
- La concentration en vitamine D par goutte est parfois très élevée (jusqu’à 10.000 UI) et les doses recommandées en fonction de l’âge ne sont pas toujours indiquées ;
- Il existe un risque d’erreur de dosage en cas de changement de complément alimentaire ou lors du passage d’un médicament à un complément alimentaire ;
- De nombreux produits avec des concentrations / dosages différents sont disponibles, parfois au sein de la même marque (risque de confusion, voire de cumul de doses, en cas d’association entre des produits contenant de la vitamine D) ;
D’autres vitamines peuvent être présentes dans le complément alimentaire. Par exemple, la vitamine K, pour laquelle il n’existe pas de recommandation pour une administration quotidienne à des enfants, ou du calcium à forte dose, qui peut aggraver le risque d’atteinte rénale (lithiase / néphrocalcinose).
Comment prévenir ce risque ?
Afin de prévenir ce risque de surdosage en vitamine D, il est recommandé de :
- Privilégier les médicaments par rapport aux compléments alimentaires, notamment chez le jeune enfant (le prescripteur choisira la spécialité pharmaceutique qu’il estime préférable à l’issue d’un échange avec les parents) ;
- Contrôler les doses administrées (vérifier la quantité en vitamine D par goutte) ;
- Ne pas multiplier les produits contenant de la vitamine D.
Une mise à jour des recommandations nationales concernant les doses de vitamine D destinées aux enfants est actuellement en cours afin de s’aligner sur les recommandations européennes :
- 400 UI par jour de 0 à 18 ans chez l’enfant en bonne santé sans facteur de risque ;
- 800 UI par jour de 0 à 18 ans chez l’enfant ayant un facteur de risque.
Il est important de rappeler aux parents que l’achat de compléments alimentaires sur Internet est déconseillé, ceux-ci pouvant ne pas être conformes à la réglementation.
Cet article a été initialement publié sur Univadis.fr, membre du réseau Medscape.
Actualités Medscape © 2021
Citer cet article: Surdosage en vitamine D : éviter les compléments alimentaires chez l’enfant – Medscape – 29 janv 2021.
La #hiperglucemia, con o sin #diabetes, triplica la mortalidad en #covid-19
El control de la glucemia junto con el de la oxigenación es esencial para evitar ingresos en UCI, ventilación mecánica y mortalidad.

Ya es bien sabido que la diabetes es uno de los principales factores de riesgo de mortalidad en covid-19, pero lo que ha ido sorprendiendo a los clínicos en estos meses es que la hiperglucemia sin diabetes también eleva la mortalidad, así como los ingresos en UCI y la ventilación mecánica.
Lo confirmó un estudio que se publicó en noviembre pasado en Annals of Medicine firmado por 25 internistas españoles encabezados por Francisco Javier Carrasco, del Hospital Juan Ramón Jiménez, de Huelva, y que se ha presentado ahora en la 15ª Reunión Virtual del Grupo de Trabajo de Diabetes, Obesidad y Nutrición de la Sociedad Española de Medicina Interna, desarrollada esta semana con la asistencia de 600 miembros de dicha sociedad.
“Todos los pacientes con covid-19 deberían evaluar su nivel de glucemia, y en caso de elevaciones consultar con su médico. Los diabéticos podrían necesitar intensificación del tratamiento en las primeras fases de la enfermedad y en los no diabéticos podría ser necesario iniciar tratamiento”, explica Carrasco a DM. La hiperglucemia -insiste- no debe pasarse por alto, con independencia de los antecedentes de diabetes.
El objetivo principal del estudio, multicéntrico y retrospectivo, era establecer la asociación entre los niveles de glucosa en sangre y la mortalidad hospitalaria en pacientes no críticos hospitalizados con covid-19. Se evaluaron datos clínicos de 11.312 pacientes, clasificándose en tres grupos, según los niveles de glucemia al ingreso: <140 mg/dl, 140-180 mg/dl y >180 mg/dl. El criterio de valoración principal fue la mortalidad hospitalaria por todas las causas.
Dos razones fisiológicas
Tras el análisis de datos y después de ajustar parámetros por edad, diabetes, hipertensión y otros factores de confusión, la probabilidad acumulada de mortalidad fue significativamente mayor en pacientes con hiperglucemia en comparación con los normoglucémicos, con independencia de la presencia de diabetes. De los 11.312 pacientes, solamente 2.128 (18,9%) tenían diabetes y 2.289 (20,4%) fallecieron durante la hospitalización. Las tasas de mortalidad hospitalaria fueron del 15,7% para pacientes con glucemia <140 mg/dl, del 33,7% para aquellos con 140-180 mg/dl y del 41,1% para pacientes con >180 mg/dl de glucemia.
“Hay al menos dos razones plausibles por las que la hiperglucemia aguda podría ser perjudicial en pacientes con covid-19”, afirma Carrasco. “Primero, el SARS-CoV-2 podría infectar las células pancreáticas a través de su expresión de la enzima convertidora de angiotensina 2 (ACE2), lo que da como resultado un deterioro de las células beta y de la secreción de insulina. En segundo lugar, la inflamación durante la covid-19 también podría generar resistencia a la insulina. Ambos mecanismos combinados podrían inducir hiperglucemia en las primeras etapas de la enfermedad y empeorar la infección”.
Es decir, la hiperglucemia, al aumentar la expresión de ACE2, el receptor que facilita la entrada del virus, induce la glicosilación de ACE2, facilitando la invasión de las células. La experiencia de estos meses de pandemia indica que un óptimo control de la glucemia favorece la recuperación y reduce la mortalidad. “Nuestro estudio -añade Carrasco- es consistente con otros de menor entidad que se han publicado y refuerza la fuerte asociación entre hiperglucemia y mortalidad intrahospitalaria en pacientes no críticos, al margen de los antecedentes de diabetes”.
Según los datos de la SEMI, la hiperglucemia aguda ocurre en el 22% de hospitalizados por covid-19, mientras que los diabéticos suponen el 18,9% de los pacientes, si bien otros registros han encontrado hiperglucemia en la mitad de los pacientes.
Desequilibrio metabólico
Una pregunta es si la hiperglucemia es un mero espectador o un protagonista del proceso inflamatorio. Aparte de la glicosilación de los receptores ACE2 que facilitan la unión del virus y el proceso inflamatorio que aumenta la resistencia a la insulina, la tan frecuente hipoxia se suele acompañar de trastornos metabólicos de la glucosa.
En condiciones anaeróbicas, explica Javier Carrasco, la glucosa se fermenta en lactato, que limita la cantidad de trifosfato de adenosina (ATP). La hipoxia y el agotamiento de ATP provocan una elevación de niveles de lactato en sangre. “En nuestro estudio, la elevación del nivel de lactato también se asoció con la mortalidad de acuerdo con los niveles de glucosa en sangre. Esta relación sugiere que un desequilibrio temprano en el metabolismo de la glucosa podría estar involucrado de manera crucial en la fisiopatología de la infección respiratoria viral. Por eso es necesario tanto el control de la oxigenación como la monitorización de la glucemia en los pacientes a los que se les solicite permanecer en casa en las primeras etapas de la infección”.
Esa detección y corrección precoz de la hiperglucemia disminuye la liberación de citocinas inflamatorias y reduce la capacidad vinculante de la ACE2. El internista del hospital de Huelva recuerda que en la primera ola no había evidencia suficiente sobre el beneficio del control glucémico estricto en pacientes con covid-19, por lo que se subestimó su importancia. “Ahora, aunque no hay ningún tratamiento milagroso, ya sabemos mejor qué fármacos ofrecen algún beneficio, como corticoides, remdesivir, plasma o tocilizumab, y cuáles no proporcionan ninguna ayuda”. En hiperglucemia, la infusión de insulina baja los niveles de dímero D e interleucina 6, dos de los marcadores básicos de la covid-19.
En este sentido, uno de los efectos, conocidos, de los corticoides, como la dexametasona, es cierta hiperglucemia. Carrasco matiza que en su mayoría los pacientes analizados no tomaban corticoides, fármaco que se ha ido imponiendo más tarde, por lo que es un factor que no ha contaminado los resultados. Sí reconoce la falta de medición en muchos de los pacientes del estudio de la hemoglobina glicosilada (HbA1c), por lo que algunos casos clasificados como no diabéticos podrían tener diabetes no diagnosticada.
En la reunión virtual de la SEMI se ha presentado un algoritmo muy práctico, dividido en tres niveles de glucemia basal y disponible en la página web de la sociedad científica, para el abordaje de la hiperglucemia hospitalaria en la covid-19, tanto para pacientes sin diabetes conocida como para diabéticos.
Más importante que la glucemia
En la 15ª Reunión Virtual del Grupo de Trabajo de Diabetes, Obesidad y Nutrición de la Sociedad Española de Medicina Interna se ha presentado además la actualización del algoritmo de tratamiento de la diabetes tipo 2, según la situación clínica del enfermo y según las cifras de hemoglobina glicosilada.
“Junto a una mejor selección de los fármacos en función de las evidencias recientes y adaptados al perfil clínico de cada paciente, la guía detalla las pautas sobre fármacos encaminadas a mejorar la insuficiencia cardiaca y a prevenir la enfermedad renal”, resume Javier Carrasco.
Se estima que entre el 25 y el 30% de los pacientes que ingresan en los servicios de Medicina Interna son diabéticos. Y hasta el 50% de los que ingresan por enfermedad cardiovascular presentan también diabetes como patología de base. “La prevalencia de la enfermedad cardiovascular en diabéticos es progresiva con la edad. Hasta el 60% de los diabéticos desde hace más de 15 años desarrollan o asocian afectación cardiovascular”.
El internista del Hospital Juan Ramón Jiménez, de Huelva, insiste en que “es esencial un tratamiento precoz y global que controle los factores de riesgo y frene la enfermedad cardiovascular. Bajar la glucemia no es lo más importante. Han de evitarse las complicaciones asociadas de carácter sistémico, como la enfermedad arterial periférica, la afectación cardíaca y renal, entre otras”.
Estudiar el patrón alimentario para entender el abuso de sustancias
Los estudios preclínicos, que no son automáticamente extrapolables a humanos, muestran resultados interesantes que abren vías de investigación en este campo.

La actividad on line Dieta y salud mental, organizada por la Escuela Europea de Pensamiento Lluís Vives de la Universidad de Valencia (UV), puso ayer martes de manifiesto que el análisis y manejo de la dieta alimentaria podría convertirse en una herramienta para abordar el abuso de sustancias, aprovechando que ambas situaciones comparten el impacto sobre el sistema cerebral de recompensa. Esta situación, que se está observando en modelos animales, también se ve acompañada por estudios clínicos y prospectivos que avalan conexiones importantes entre el tipo de dieta y trastornos mentales.
María del Carmen Blanco Gandía, doctora en Psicología por la UV y profesora ayudante doctora en la Universidad de Zaragoza, expuso sus investigaciones centrada en el estudio del papel de la dieta como factor de vulnerabilidad o protección en el consumo de drogas con modelos animales. Como punto de partida, recordó que el ser humano, a través del sistema cerebral de recompensa, tiende a repetir conductas que experimentamos naturalmente como placenteras (comer, beber, dormir, sexo/reproducción…) y las drogas de abuso, que surgen como “un intruso” en este esquema y, “hacen creer a nuestro cerebro que son necesarias para sobrevivir”.
A través de animales de experimentación y manejando una dieta palatable de forma intermitente y continuada, la investigadora ha podido contrastar respuestas de gran interés. Por ejemplo, según expuso en su charla, mientras se consume este tipo de comida de forma continuada, “nuestro sistema de recompensa cerebral se encuentra saciado”, pero cuando cesa esta, aumenta la vulnerabilidad ante las sustancias y la ingesta de drogas o alcohol. Dado que este tipo de alimentación puede tener consecuencias para la salud, también se ha estudiado la posibilidad de dar comida palatable “de forma puntual”. Y los resultados muestran que puede desplazar la recaída totalmente en machos y de forma parcial en hembras. En este contexto, comentó que la dieta cetogénica está dando “resultados bastante prometedores”.
Para confirmar el binomio alimentación-abuso de sustancias, Blanco Gandía señaló que diversos estudios muestran que los pacientes con trastorno por uso de sustancias (TUS) “muestran mayores puntuaciones en cuestionarios de trastornos de conducta alimentaria (TCAs)” o que usan “la comida para satisfacer el ansia por la droga, especialmente en los primeros seis meses de sobriedad”.
Asimismo, las personas con TUS tienen alta preferencia por los ultraprocesados, ya que presentan un “dosis alta” de recompensa y absorción rápida, que podría equivaler a las propias drogas.
A modo de conclusión, recordó que los estados emocionales negativos “nos empujan a buscar consuelo en la comida”, señalando que esta no sería “un tratamiento único” para el abuso de sustancias, pero sí podría convertirse en “un pilar crucial”.
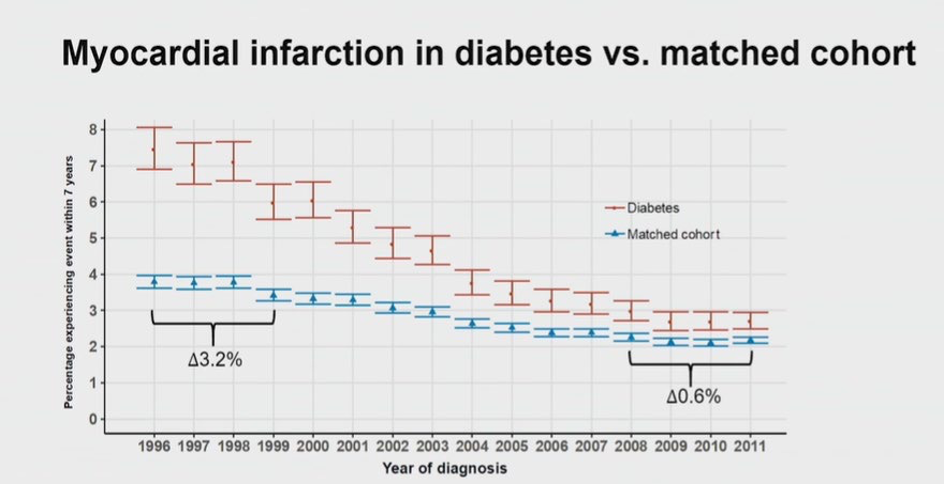
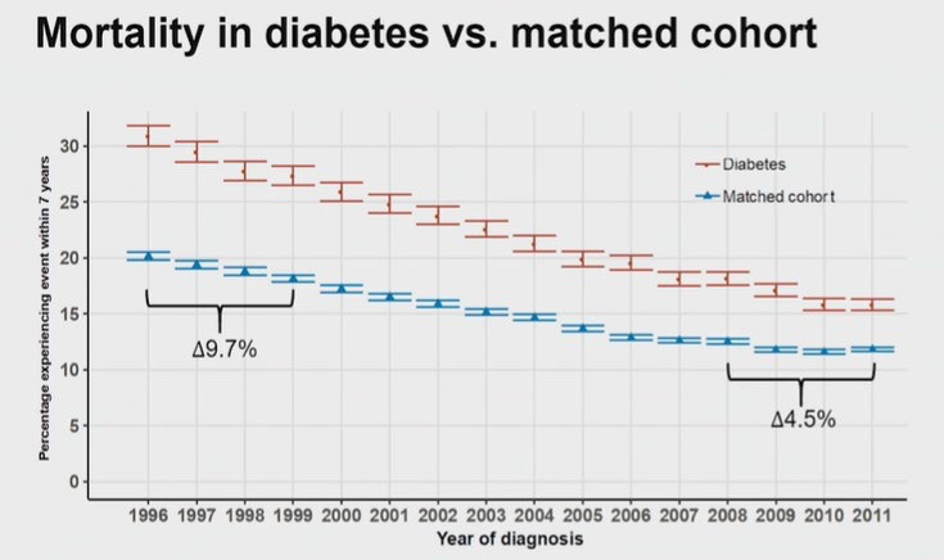
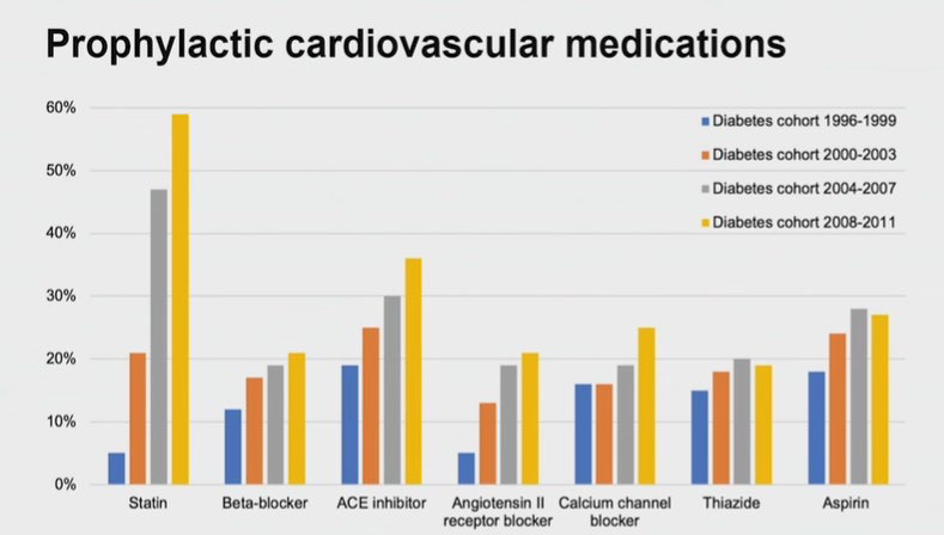
Bonne nouvelle : le diabète n’est plus un facteur de risque d’infarctus du myocarde ?

Bernard BAUDUCEAU, Hôpital d’Instruction des Armées Bégin, Saint-Mandé
Ce titre provoquant se fonde sur l’exploitation des données des registres danois qui montrent une diminution régulière et spectaculaire de l’incidence des infarctus du myocarde et de la mortalité chez les patients diabétiques. Ces chiffres rejoignent presque ceux d’une population témoin comme le montrent les résultats présentés lors de l’ESC en 2020. Pourtant, l’incidence des complications cardiovasculaires, et notamment de l’infarctus du myocarde est habituellement considérée comme majorée d’un facteur 2 à 3 chez les patients diabétiques.
Cette étude de suivi a été menée grâce au croisement des données des registres danois portant sur le diabète et la maladie coronarienne. La cohorte étudiée se composait de patients ayant fait l’objet d’une coronarographie entre 2003 et 2012. Ces sujets ont été stratifiés en fonction de l’existence d’une maladie coronarienne et d’un diabète. Les critères d’évaluation comprenaient la survenue d’un infarctus du myocarde, de la réalisation d’une revascularisation coronarienne, d’un décès d’origine cardiaque ou de la mort toutes causes confondues.
Au total, 86 202 patients dont 12 652 personnes diabétiques ont été inclus et ont fait l’objet d’un suivi médian de 8,8 ans. En prenant pour référence les patients ne présentant ni maladie coronarienne ni diabète dont l’incidence cumulée d’infarctus du myocarde était 2,6 %, ce risque n’était que très discrètement majoré à 3,2 % chez les patients diabétiques sans coronaropathie (HR = 1,202 ; IC 95% : 0,996-1,451). Cette incidence de la survenue d’un infarctus du myocarde était augmentée et atteignait 9,3 % chez les patients atteints de coronaropathie sans diabète associé (HR = 2,75 ; IC95% : 2,52-3,01) et était la plus élevée à 12,3 % chez les patients atteints à la fois de maladie coronarienne et de diabète (HR = 3,79 ; IC95% : 3,43-4,20). Des résultats similaires ont été observés pour la fréquence de la mort d’origine cardiaque et de la revascularisation coronarienne.
Ainsi dans cette étude, les patients diabétiques sans coronaropathie authentifiée par une coronarographie ont un faible risque d’infarctus du myocarde qui n’est pas sensiblement augmenté par rapport aux patients sans coronaropathie ni diabète. Cependant, en présence d’une maladie coronarienne, le diabète majore nettement le risque d’infarctus du myocarde. Ces résultats très satisfaisants témoignent de l’amélioration de la prise en charge des patients diabétiques et coïncident avec l’utilisation plus régulière et plus fréquente des médicaments ayant fait la preuve de leur efficacité dans la protection cardiovasculaire.
Publié par Diabétologie Pratique
Références
Cliquez sur les références et accédez aux Abstracts sur 
Gyldenkerne C et al. Diabetes is not a risk factor for myocardial infarction in patients without coronary artery disease: a study from the Western Denmark Heart Registry. Diab Vasc Dis Res 2020 ; 17 : 1479164120941809. Rechercher l’abstract
Widespread Liver Disease Missed in Patients With Type 2 Diabetes

Dr Christos S. Mantzoros
Mounting evidence of strikingly high prevalence rates of fatty liver disease, advanced fibrosis, and cirrhosis among patients with type 2 diabetes has led to calls for heightened awareness and screening to identify these patients and target treatments to reduce their risk for irreversible liver damage.
Among these calls is a pending statement from the Endocrine Society, the American Association of Clinical Endocrinologists, the American Gastroenterology Association, and other groups on what the growing appreciation of highly prevalent liver disease in patients with type 2 diabetes (T2D) means for assessing and managing patients. Publication of the statement is expected by spring 2021, said Christos S. Mantzoros, MD, DSc, PhD, chief of endocrinology for the Veterans Affairs Boston Healthcare System and a representative from the Endocrine Society to the statement-writing panel.
This upcoming “Call to Action” from these groups argues for a “need to collaborate across disciplines, and work together on establishing clinical guidelines, and creating new diagnostics and therapeutics,” said Mantzoros in an interview.
“Over time, it is becoming clearer that management of NAFLD [nonalcoholic fatty liver disease]/NASH [nonalcoholic steatohepatitis] requires a multidisciplinary panel of doctors ranging from primary care practitioners, to endocrinologists, and hepatologists. Given that the nature of the disease crosses scientific discipline boundaries, and that the number of patients is so large (it is estimated that about one in four U.S. adults have NAFLD), not all patients can be treated at the limited number of hepatology centers.
“However, not all stakeholders have fully realized this fact, and no effort had been undertaken so far by any professional society to develop a coordinated approach and clinical care pathway for NAFLD/NASH. The ‘Call to Action’ meeting can be considered as a starting point for such an important effort,” said Mantzoros, who is also a professor of medicine at Harvard Medical School and director of the human nutrition unit at Beth Israel Deaconess Medical Center, both in Boston.
Dramatic Prevalence Rates in Patients With T2D
Results from two independent epidemiology reports, published in December 2020, documented steatosis (the fatty liver of NAFLD) in 70%-74% of unselected U.S. patients with T2D, advanced liver fibrosis accompanying this disease in 6%-15%, and previously unrecognized cirrhosis in 3%-8%.https://9f5ac8ceeb5230fa64f15927ee9552c7.safeframe.googlesyndication.com/safeframe/1-0-37/html/container.html
One of these reports analyzed 825 patients with T2D included in the National Health and Nutritional Examination Survey of 2017-2018 run by the Centers for Disease Control and Prevention. All these patients, selected to be representative of the overall U.S. adult population with T2D, underwent transient elastography to identify steatosis and fibrosis, the first U.S. National Health Survey to run this type of population-based survey. The results showed an overall steatosis prevalence of 74% with grade 3 steatosis in 58%, advanced liver fibrosis in 15%, and cirrhosis in 8%, reported the team of Italian researchers who analyzed the data.
Dr Kenneth Cusi
Neither report documented a NASH prevalence, which cannot receive definitive diagnosis by imaging alone. “This is the first study of its kind in the U.S. to establish the magnitude of [liver] disease burden in random patients with T2D seeking regular outpatient care,” wrote the University of Florida research team, led by Kenneth Cusi, MD, professor and chief of the university’s division of endocrinology, diabetes, and metabolism. Their finding that patients with T2D and previously unknown to have NAFLD had a 15% prevalence of moderate or advanced liver fibrosis “should trigger a call to action by all clinicians taking care of patients with T2D. Patient and physician awareness of the hepatic and extrahepatic complications of NASH, and reversing current diagnosis and treatment inertia will be the only way to avert the looming epidemic of cirrhosis in patients with diabetes.”
“Endocrinologists don’t ‘see’ NAFLD and NASH” in their patients with T2D ” because they don’t think about it,” Mantzoros declared.
“Why is NASH underdiagnosed and undertreated? Because many physicians aren’t aware of it,” agreed Cusi during a talk in December 2020 at the 18th World Congress on Insulin Resistance, Diabetes, and Cardiovascular Disease (WCIRDC). “You never find what you don’t look for.”
“Endocrinologists should do the tests for NASH [in patients with T2D], but we’re all guilty of not doing it enough,” Tracey McLaughlin, MD, an endocrinologist and professor of medicine at Stanford (Calif.) University, commented during the WCIRDC.
These prevalence numbers demand that clinicians suspect liver disease “in any patient with diabetes, especially patients with obesity who are older and have components of metabolic syndrome,” said Mantzoros. “We need to screen, refer the most advanced cases, and treat the early- and mid-stage cases.”
How to Find NASH
Both the American Diabetes Association and the European Association for the Study of Diabetes call for routine screening of patients with T2D, starting with a check of liver enzymes, such as ALT, but no clear consensus exists for the specifics of screening beyond that. Mantzoros, Cusi, and other experts agree that the scheme for assessing liver disease in patients with T2D starts with regular monitoring of elevations in liver enzymes including ALT. Next is noninvasive ultrasound assessment of the extent of liver fibrosis inferred from the organ’s stiffness using transient elastography. Another frequently cited initial screening tool is the Fibrosis-4 (FIB-4) score, which incorporates a patient’s age, platelet count, and levels of ALT and a second liver enzyme, AST.
“There is more consensus about FIB-4 and then elastography, but some people use tests other than FIB-4. Unfortunately there is no perfect diagnostic test today. A top priority is to define the best diagnostic test,” said Mantzoros, who is leading an effort to try to refine screening using artificial intelligence.
“FIB-4 is simple, easy, and well validated,” commented Cusi during the WCIRDC last December. “FIB-4 and elastography should get you pretty close” to identifying patients with T2D and significant liver disease.
But in a recent editorial, Cusi agreed on the need for “more reliable tests for the diagnosis of NASH and advanced fibrosis in patients with T2D. Significant work is being done in the field to validate novel and more sophisticated fibrosis biomarkers. Future studies will help us enter a new era of precision medicine where biomarkers will identify and target therapy to those with more active disease at risk for cirrhosis,” he wrote.
“The ultimate goal is to diagnose fibrosis at an early stage to prevent people from developing cirrhosis,” Cusi said in a recent written statement. “We’re trying to identify these problems before they’re unfixable. Once someone has cirrhosis, there isn’t a whole lot you can do.”
Pioglitazone Remains the Best-Documented Treatment
Perhaps some of the inertia in diagnosing NAFLD, NASH, and liver fibrosis in patients with T2D is dissatisfaction with current treatment options, although several proven options exist, notably weight loss and diet, and thiazolidinedione (TZD) pioglitazone. But weight loss and diet pose issues for patient compliance and durability of the intervention, and many clinicians consider pioglitazone flawed by its potential adverse effects.
“When we don’t have an established treatment for something, we tend to not measure it or go after it. That’s been true of liver disease” in patients with T2D, said Yehuda Handelsman, MD, an endocrinologist and diabetes specialist who is medical director of the Metabolic Institute of America in Tarzana, Calif., during the WCIRDC.
Treatment with pioglitazone has resolved NASH in about a third of patients compared with placebo, prevented fibrosis progression, and cut cardiovascular disease events, noted Cusi during the WCIRDC.
“Pioglitazone is used in only 8% of patients with T2D, or less, but we need to use it more often because of its proven efficacy in patients with T2D and NASH” said Mantzoros. “The problem is that pioglitazone has side effects, including weight gain and fluid retention, that makes it less attractive unless one thinks about the diagnosis of NASH.”
Dr Ralph A. DeFronzo
“The data with the TZDs are much stronger than the data from anything else. TZDs have gotten a bad name because they also work in the kidney and enhance fluid reabsorption. We use modest dosages of pioglitazone, 15 mg or 30 mg a day, to avoid excess fluid retention,” Ralph A. DeFronzo, MD, chief of the diabetes division and professor of medicine at the University of Texas Health Science Center, San Antonio, said during the WCIRDC. “The best drug for NASH is pioglitazone. No other drug beats it” based on current data, DeFronzo asserted.
Other strategies include the potential to pair pioglitazone with other interventions that can blunt a weight-gain effect. One intriguing combination would combine pioglitazone with a GLP-1 receptor agonist, a drug class that can produce significant weight loss. Results from a phase 2 study showed promise for semaglutide (Rybelsus) in treating patients with NASH.
Getting the Name Right
Another factor that may be keeping NAFLD and NASH from achieving a higher profile for patients with T2D are those names, which focus on what the diseases are not – nonalcoholic – rather than what they are.
A series of recent publications in both the endocrinology and hepatology literature have called for renaming these disorders either “metabolic (dysfunction)–associated fatty liver disease (MALFD)”, or “dysmetabolism-associated fatty liver disease (DALFD)”.
“The names NAFLD and NASH indicate absence of alcohol as a cause, but the disease is also characterized by the absence of other causes, such as autoimmune disorders or hepatitis. The names were coined when we did not know much about these diseases. We now know that it is dysmetabolism that causes these conditions, and so we need to adopt a new, more accurate name,” explained Mantzoros, who has published support for a name change.
While many agree, some have raised concerns as to whether a name change now is premature. A group of hepatologists recently published a rebuttal to an immediate name change, saying that, “although we are in agreement that metabolic fatty liver disease may more accurately and positively reflect the relevant risk factors better than the age-old term nonalcoholic fatty liver disease, the term still leaves a great deal of ambiguity. A name change will be appropriate when informed by a new understanding of the molecular basis of the disease entity, insights that fundamentally change risk stratification, or other important aspects of the disease. We may be on the cusp of this, but we are not there yet.”
Mantzoros agreed, but for somewhat different reasons.
“We need to be careful and deliberate, because there is a significant body of knowledge and a lot of data from clinical trials collected using the old definitions. We need to find an appropriate time frame for a [name] transition. We need to find a nice and robust way to productively bridge the old to the new,” he said. “We also need new diagnostic criteria, and new therapies. A new name and definition will facilitate progress.”
Mantzoros been a shareholder of and consultant to Coherus and Pangea, he has been a consultant to AstraZeneca, Eisai, Genfit, Intercept, Novo Nordisk, P.E.S., and Regeneron, and has received travel support from the Metabolic Institute of America and the California Walnut Commission. Cusi has been a consultant to and has received research funding from numerous drug companies. McLaughlin is a consultant to January AI. Handelsman has been a consultant to numerous drug companies. DeFronzo received research grants from AstraZeneca, Janssen, and Merck; he has been an adviser to AstraZeneca, Boehringer Ingelheim, Intarcia, Janssen, and Novo Nordisk; and he has been a speaker on behalf of AstraZeneca and Novo Nordisk.
This article originally appeared on MDedge.com, part of the Medscape Professional Network.
Medscape Medical News © 2021 WebMD, LLC
Cite this: Widespread Liver Disease Missed in Patients With Type 2 Diabetes – Medscape – Jan 25, 2021.
COVID-19 chez les diabétiques : nouvelles données sur les facteurs de risque

France — Une étude écossaise de large envergure montre que par rapport aux sujets non diabétiques, ceux souffrant de diabète de type 1 et de type 2 étaient respectivement 2,4 fois et 1,4 fois plus à risque d’être orientés vers une unité de soins intensifs ou de décéder du SARS-CoV-2. Les résultats ont été publiés dans le Lancet Diabetes Endocrinol[1].
Les auteurs suggèrent que la majoration du risque chez les DT1 par rapport aux DT2 pourrait être liée à une durée plus importante du diabète. Cette étude a révélé de nouveaux facteurs de risque de Covid-19 grave ou fatal, notamment l’admission hospitalière dans les 5 dernières années pour cause d’hypoglycémie ou d’acidocétose diabétique, le tabagisme, le traitement par plusieurs anti-diabétiques.
Etude de cohorte dans la population écossaise
Cette étude de cohorte est basée sur les données liées à la première vague d’épidémie à SARS-CoV-2 en Écosse entre le 1er mars 2020 et le 31 juillet 2020. Les analyses ont porté sur l’ensemble de la population écossaise en vie 3 semaines avant le début estimé de la pandémie fixé au 7 février 2020. Le statut diabétique était obtenu à partir du registre national du diabète. Ce registre ainsi que les bases de données administratives ont permis de rechercher des facteurs de risque de COVID-19 grave ou fatal.
Au 1er mars 2020, la population écossaise comptait 5,4 millions d’individus, dont 5,8% de diabétiques (n = 319 349). Parmi ces derniers, 0,3% sont décédés ou ont nécessité des soins intensifs pour cause de Covid-19, contre 0,1% chez ceux qui n’avaient pas de diabète. Seuls 2,8% des sujets diabétiques ayant une forme grave ou fatale de Covid-19 étaient âgés de moins de 50 ans et 89,8% avaient 60 ans et plus.
Plusieurs facteurs de risque ont été mis en évidence
L’âge, le sexe masculin et la durée du diabète se sont révélés être des facteurs significatifs d’augmentation de risque de Covid-19 grave ou fatal. Par rapport aux sujets non diabétiques, ceux souffrant d’un diabète de type 1 avaient un risque de Covid-19 grave ou fatal plus que doublé (odds ratio : 2,396) et ceux atteints de diabète de type 2, un risque augmenté de 37%. Après ajustement sur l’âge, le sexe, la durée du diabète, plusieurs facteurs de risque ont été mis en évidence, notamment : le sexe masculin, la vie en établissement de soins ou dans une zone défavorisée, la présence d’une comorbidité reconnue à risque de Covid-19, la rétinopathie, la diminution de la fonction rénale, un mauvais contrôle glycémique, ainsi que le fait avoir des antécédents d’hospitalisation pour acidose diabétique ou hypoglycémie dans les 5 dernières années, d’être traités par plusieurs anti-diabétiques ou autres traitements ou bien encore d’être fumeur. En période de forte épidémie, l’identification de ces facteurs est importante afin d’inciter les sujets concernés à être encore plus vigilants dans leur vie quotidienne.
Ce type d’étude n’est pas sans biais, soulignent les auteurs. On peut, par exemple, s’attendre à ce que les sujets diabétiques aient plus adopté les mesures de distanciation sociale que les non-diabétiques, ce qui pourrait avoir impacté à la baisse le risque de Covid-19 grave ou fatal.
Actualités Medscape © 2021 WebMD, LLC
Citer cet article: COVID-19 chez les diabétiques : nouvelles données sur les facteurs de risque – Medscape – 21 janv 2021.
Fatores reprodutivos estão associados ao risco de fraturas no pós-menopausa?

A osteoporose é uma epidemia silenciosa, estima-se que o risco de fratura por osteoporose no mundo seja o mesmo de um acidente cardiovascular. E quando falamos especificamente de mulheres na pós-menopausa, esse risco se multiplica.
Sabemos que o estrogênio é um grande fator protetor da massa óssea. Muitos estudos já demonstraram que a idade da menarca e menopausa estão associadas à densidade mineral óssea na pós-menopausa: quanto mais precoce a menarca e/ou mais tarde a menopausa, menor o risco de fraturas osteoporóticas futuras devido ao maior tempo de exposição ao estrogênio.
Novos estudos
Nestas últimas semanas, o JAMA publicou um novo estudo, uma coorte de base populacional de 1.272.115 mulheres coreanas investigando se os fatores reprodutivos femininos isoladamente estão associados a fraturas em mulheres na pós-menopausa.
Foram então avaliados: idade na menarca, idade na menopausa, paridade, amamentação e uso de hormônio exógeno, a partir questionário autoaplicável. E, então, esses dados foram relacionados a incidência fraturas vertebrais, quadril e outros sítios osteoporóticos.
A média de idade da população do estudo foi de 61,0 anos. A média geral de idade na menarca foi de 16,4 anos e na menopausa foi de 50,1 anos. O período reprodutivo médio foi de 33,6 anos. Em comparação com mulheres sem fraturas (n = 1.082.232), as mulheres com fratura incidente (n = 189.883) eram provavelmente mais velhas (idade média, 63,7 vs 60,5 anos), multíparas ( 92,8% vs 91,0%), menarca tardia (média idade na menarca, 16,7 vs 16,4 anos), menopausa precoce (idade média na menopausa, 49,9 vs 50,1 anos), um período reprodutivo mais curto (33,3 vs 33,7 anos) e uma duração da amamentação de 12 meses ou mais (74,0% vs 67,8%) e nunca ter usado terapia hormonal(82,6% vs 80,1%) ou anticoncepcional oral (80,0% vs 79,8%).
Paridade e risco de fraturas osteoporóticas
O aumento da paridade está associado a uma redução no risco de fratura osteoporótica entre as mulheres na pós-menopausa. Os níveis séricos de estrogênio aumentam muito durante a gravidez para níveis aproximadamente 20 a 30 vezes acima de seu pico durante o ciclo menstrual normal. Essa exposição acentuada ao estrogênio durante cada gravidez pode reduzir o risco de fratura da mulher.
O estudo propõe também que algumas mulheres nulíparas podem ser “subférteis”, produzindo menos estrogênio durante o ciclo menstrual do que as mulheres mais férteis e, portanto, apresentam maior risco de fratura.
Foi observado que as mulheres primíparas tiveram um risco menor de todas as fraturas do que as mulheres nulíparas, mas a multiparidade não mostrou uma associação significativa com o risco de qualquer fratura.
Amamentar pode reduzir risco de fratura de quadril e aumentar risco de fratura de demais sítios
Embora se acredite que a perda óssea durante a lactação seja restaurada 6 a 12 meses após o desmame por mecanismos pouco conhecidos, o estudo propõe que a duração prolongada do aleitamento materno aumenta o risco de qualquer fratura, bem como de fratura vertebral.
No entanto, também foi observado um risco reduzido de fratura de quadril em mulheres que amamentaram comparado às que não. Uma metanálise publicada em janeiro de 2020 já havia relatado que a incidência de fratura de quadril osteoporótica diminuiu com a extensão do tempo de amamentação. Outros pesquisadores relataram uma associação entre maior duração da lactação e menor DMO na coluna lombar, mas não no colo femoral ou no quadril total.
A perda esquelética é mais profunda no osso trabecular do que no osso cortical durante a lactação: a vértebra é composta, principalmente, de osso trabecular, enquanto quadril é em grande osso cortical. O osso trabecular é mais metabolicamente ativo do que o osso cortical, e então, mais suscetível do que o osso cortical a influências hormonais e reduções na reserva de cálcio.
Pílula e risco de fratura osteoporótica
Os anticoncepcionais orais combinados também podem melhorar a densidade óssea por mecanismos biologicamente plausíveis, mas existe uma controvérsia considerável nesse assunto. Apesar de outros estudos demonstrarem essa associação positiva, este trabalho atual surpreendentemente revelou um achado pequeno, porém estatisticamente significante de um risco aumentado de fraturas entre aquelas pacientes que haviam usado pílula combinada por 1 ano ou mais.
Por fim, este estudo constatou que os fatores reprodutivos femininos foram independentemente associados à incidência de fraturas entre as mulheres na pós-menopausa
Até o momento, este foi o maior estudo que avaliou associação de fatores reprodutivos femininos com risco de fratura. A ferramenta de risco de fratura da Organização Mundial da Saúde (FRAX) é a mais utilizado para estimar fraturas osteoporóticas, integrando fatores de risco clínicos, mas ainda não inclui fatores reprodutivos,
Espera-se que esses fatores sejam incorporados aos algoritmos existentes conforme mais dados adicionais estejam disponíveis.
Autor(a):
Juliana Olivieri
Graduada em Medicina pela Universidade Federal do Rio de Janeiro (UFRJ) ⦁ Ginecologista e Obstetra ⦁ Pós-graduada em Endocrinologia Feminina e Climatério pelo Instituto Nacional de Saúde da Mulher da Criança e do Adolescente Fernandes Figueira(IFF/Fiocruz)
Referências bibliográficas:
- Yoo JE, Shin DW, Han K, Kim D, Yoon JW, Lee D. Association of Female Reproductive Factors With Incidence of Fracture Among Postmenopausal Women in Korea. JAMA Netw Open.2021;4(1):e2030405. doi:1001/jamanetworkopen.2020.30405