tecnología
Interação entre telefones celulares e CDI
Arritmias ventriculares graves, que geralmente trazem risco de morte, são grande parte das vezes tratadas com cardioversores-desfibriladores implantáveis (CDI), que são compostos, de forma simplificada, por uma bateria, capacitores e um circuito de sensing/pacing. O sistema embutido no dispositivo responde a um campo magnético aplicado externamente e quando isso ocorre a terapia de choque fica suspensa temporariamente, ou seja, o aparelho não dará o choque se o paciente apresentar fibrilação ou taquicardia ventricular.
O novo aparelho iPhone 12, lançado recentemente, apresenta uma matriz circular de ímãs ao redor de uma bobina central, que faz com que seja compatível com acessórios MagSafe e possa ser realizado carregamento sem fio, de forma rápida, entre outras funções.

Interação entre as tecnologias
Recentemente houve relatos de possível interação do telefone com aparelhos de CDI que seria decorrente de um forte campo magnético gerado pelo Iphone e tecnologia MagSafe. Isso foi confirmado em experimento em que o telefone foi aproximado da região torácica esquerda de paciente com CDI e houve suspensão imediata das terapias do aparelho, que persistiu durante todo o teste. Esse experimento foi reproduzido diversas vezes com o telefone em diferentes posições, com o mesmo efeito. Aparelhos mais antigos não tem essa capacidade.
Também foi feito experimento randomizado de forma cega, com crossover que comparou o iPhone 12 com o iPhone XS (que não contém a tecnologia MagSafe). Os telefones eram colocados em envelopes, aproximados a menos de 2 cm do CDI por pelo menos 30 segundos e era feita avaliação do CDI. Não houve interação do iPhone XS com o CDI, porém o iPhone 12 causou suspensão da detecção de arritmias e inibição da terapia em dispositivos de diferentes marcas. Além disso, fez com houvesse reprogramação do marca-passo para modo assíncrono em um aparelho de marca específica.
Conclusão
As consequências da interação de telefones com essa nova tecnologia e aparelhos de CDI podem ser catastróficas. Como maneira de prevenir que isso ocorra, devemos reforçar ainda mais aos pacientes que usam esses dispositivos que não devem colocar os telefones próximos ao CDI, assim como qualquer outro dispositivo eletrônico que possa ter potencial de causar alterações semelhantes.
Autor(a):
Isabela Abud
Editora de cardiologia do Portal PEBMED ⦁ Graduação em Medicina pela Escola Paulista de Medicina da Universidade Federal de São Paulo (UNIFESP) ⦁ Residência em Clínica Médica pela UNIFESP ⦁ Residência em Cardiologia pelo Instituto do Coração (InCor) do Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (USP) ⦁ Atualmente atuando nas áreas de terapia intensiva, cardiologia ambulatorial, enfermaria e em ensino médico.
Referências bibliográficas:
- Greenberg JC, et al. Letter to the Editor—Lifesaving Therapy Inhibition by Phones Containing Magnets. 2021 Jan 5;S1547-5271(20)31227-3. doi: 1016/j.hrthm.2020.12.032.
- Patterson Z, et al. Letter to the Editor: New phones, old problem? Interference with cardiovascular implantable electronic devices by phones containing magnets. Heart Rhythm. 2021 Feb 2;S1547-5271(21)00105-3. doi: 1016/j.hrthm.2021.01.029.
Los nuevos termómetros también necesitarán ser interpretados
Por muchas novedades que se introduzcan, con mediciones más rápidas, fiables y cómodas, la interpretación final de ese dato siempre recaerá (o debería) en un profesional sanitario.

Los termómetros son productos sanitarios clase IIa y, como ocurre en otros ámbitos biomédicos y sanitarios, los avances que pronostican los expertos consultados por CF se basan en una mejora en la conectividad con otros dispositivos o sistemas personales y/o médicos, lo cual redundaría en un mayor y mejor control de la temperatura. Además, se incrementarían las opciones a la hora de manejar los datos recogidos y acumulados. Sin embargo, también se hace hincapié en que existen múltiples aspectos que condicionan la lectura e interpretación de los valores, lo cual hace imprescindible que sean manejados por profesionales sanitarios.
Tradicionalmente, recuerdan Augusto Ortega Jiménez y Sagrario Pérez de Agreda Galiano, farmacéuticos del Centro de Información del Medicamento (CIM) del COF de Ciudad Real, se han venido utilizando termómetros de vidrio, ahora sin mercurio, y termómetros electrónicos, que utilizan sensores de temperatura en la punta metálica. Como ventajas “presentan su fácil manejo y su precisión cuando se usan correctamente y, como inconveniente, está el tiempo necesario para dar una lectura correcta”.
Pero en los últimos tiempos, y potenciados aún más por la pandemia de la Covid-19, se ha incrementado de forma notable el manejo de los termómetros infrarrojos, “que captan el calor corporal en forma de energía infrarroja desprendida por una fuente de calor”. Los farmacéuticos apuntan que “pueden ser de oído o frontales” y tienen la gran ventaja de la rápida medición y dan, además, “resultados muy fiables”.
Para Víctor Pedrera, médico de familia con más de treinta años de experiencia en Atención Primaria en Alicante, lafiabilidad de estos dispositivos es completa, e incluso mayor que la de los tradicionales termómetros de mercurio, “al dar una medición más exacta, rápida y cómoda para la consulta diaria”.
Productos esenciales
En las circunstancias actuales, en las que el distanciamiento y las medidas de prevención de contagios son si cabe aún más importantes, estos dispositivos “son esenciales”, ya que la medición de la temperatura es un dato imprescindible en el manejo del paciente “y el no contacto con el mismo permite su uso sin necesidad de desinfección de forma continuada”.
Esta ventaja es extensible al manejo del termómetro en casa, aunque Pedrera recuerda que el empleo e interpretación de esa información debe servir para que se facilite al facultativo el control y seguimiento de los problemas de salud de la población. “Nunca deben interpretar esa información y, mucho menos tomar decisiones en cuestiones de salud, personas no formadas”, insiste.
Cabe recordar que la temperatura normal no es un parámetro fijo: “La normalidad oscila entre un pequeño intervalo y puede variar por situaciones fisiológicas, ejercicio físico, temperatura exterior, momento de la comida, hora del día, etc., además de por procesos patológicos que pueden aumentarla o disminuirla”, enumera Pedrera.
También están los termómetros químicos o de cambio de fase. “Permiten un control de la temperatura gracias a que tienen sustancias químicas fotosensibles que cambian de color al variar la temperatura”, apuntan desde el CIM. Se trata de un método muy rápido y no invasivo, “pero que presenta lecturas poco exactas”.
Según los miembros del CIM del COF de Ciudad Real, las mejoras vendrán por la conectividad con otros dispositivos, lo que permitirá registrar y establecer una monitorización de la temperatura en tiempo real, o bien poder establecer mapas de temperaturas corporales”. Otra de las mejoras será la incorporación de los sensores de temperatura a smartphones y/o relojes deportivos, pulseras de actividad, etc., “para medir en cualquier momento la temperatura corporal”.
La seguridad del infrarrojo
Durante el peor momento de la pandemia de la Covid-19, aparecieron informaciones, sobre todo en cadenas de whastapp, que alertaban sobre los peligros asociados al manejo de los termómetros infrarrojos. De hecho, incluso la Sociedad Española de Neurología (SEN) tuvo que salir al paso y aclarar que los termómetros pistola no provocaban daños neurológicos ni tampoco “mataban neuronas”. También insistieron en que no causaban problemas a la vista. Para Pedrera todos esos bulos, que desgraciadamente abundan en las redes sociales, “carecen de base científica y está más que demostrado que son dispositivos seguros y exentos de efectos nocivos sobre la salud del usuario”.
Mucho se ha hablado, por supuesto no en foros científicos ni profesionales, del efecto de la radiación emitida por estos aparatos, “cuando, al contrario, lo que hacen es recoger la radiación emitida por el paciente y así medir la temperatura”. Difícil es entender que, sin emitir ningún tipo de radiación, puedan producir efectos por emisión de radiaciones.
Mascarillas ‘made in Spain’ antibióticas y biodegradables
Científicos y empresarios han aunado fuerzas para desarrollar mascarillas con un nivel de seguridad a prueba de los diminutos coronavirus.

La palabra del año en inglés según los expertos del famoso diccionario Webster es pandemic (pandemia), pero muy bien podría haber sido mask, mascarilla. Es el símbolo externo y universal de la invisible pandemia. Circunscrita hasta hace unos meses a algunos asiáticos responsables para protegerse de la contaminación o para no contagiar a los demás de sus resfriados, hoy es una prenda obligatoria en muchos países. Su escasez inicial ha dado paso a un próspero sector que ha inundado farmacias, supermercados y puestos callejeros de mascarillas de todos los colores y calidades.
El uso masivo de esta protección respiratoria de vida efímera se vislumbró enseguida como una nueva carga medioambiental, paralela a la de las toallitas higiénicas que tantos atascos causan en los desagües y colectores urbanos.
En este escenario, Bioinicia, una spin-off del Consejo Superior de Investigaciones Científicas (CSIC), decidió desarrollar en abril la primera mascarilla biodegradable certificada. Sin sacrificar en ningún momento la respirabilidad, el confort ni la eficacia -filtración bacteriana superior a un 92% y de aerosoles mayor a un 85%-, tiene la ventaja de degradarse como la materia orgánica.
Según José María Lagarón, del Instituto de Agroquímica y Tecnología de Alimentos (IATA)-CSIC y director del equipo que ha desarrollado junto con la empresa Bioinicia el filtro de nanofibras Proveil-Biomask, la necesidad de reducir esa previsible contaminación plástica les orientó a buscar filtros de nanofibras, que ofrecen una filtración mecánica, no electrostática y, según la literatura científica, presentan una morfología uniforme con tamaño de poro muy inferior al de los filtros convencionales de polipropileno meltblown. Esto permite que el aire, con tamaño aproximado de 4 nm, pueda pasar a través del filtro, a la vez que evita aerosoles virales, bacterias y partículas en suspensión.
Mediciones terrestres y marinas
Las mediciones realizadas revelan que esos filtros de nanofibras no obstruyen tanto la respiración, ya que disipan mejor el calor, la humedad y el CO2 que los filtros tradicionales de polipropileno meltblown. El equipo que lidera Lagarón, formado por Cristina Prieto, María Pardo, Álvaro Lafraya y Alberto Chiva, ha desarrollado así un filtro ultrafino y 100% compostable, salvo el clip nasal de acero inoxidable y las gomas de sujeción. Además, se puede desinfectar con pulverizaciones de solución alcohólica al 70 por ciento sin perder sus capacidades óptimas de filtración.
La Unidad Asociada del CSIC en Tecnología de Polímeros, que se encuentra en la Universidad Jaume I de Castellón, dirigida por Luis Cabedo, del Departamento de Ingeniería de Sistemas y Diseño, ha sido la encargada de estudiar los niveles de biodegradación de la Biomask, con la colaboración del Instituto de Medio Ambiente y Ciencias Marinas de la Universidad Católica de València.
El equipo formado por Cabedo, José Gámez, Patricia Feijóo, Anna Marín y Estefanía Sánchez, ha analizado la biodegradabilidad de las mascarillas en el medio terrestre y marino con pruebas de laboratorio y también en condiciones reales. Han comprobado así que no se generan microplásticos y que todo el material se transforma en CO₂ y agua, y también han medido en el medio marino su biodegradación en las instalaciones de la costa mediterránea que la UCV tiene en Calpe. Según José María Lagarón, ahora trabajan en el desarrollo de filtros a partir de residuos agroalimentarios y también se van a hacer en formato EPI “con un nivel de protección aún mayor”.
Con un minuto basta
En este nuevo campo científico y comercial, en el que la improvisación inicial con sus corredores aéreos para traer material de China ha sido sustituida por unas exigencias de control más estrictas sujetas a las normativas de la Unión Europea, otro equipo del Grupo de Biomateriales y Bioingeniería del Centro de Investigación Traslacional San Alberto Magno (CITSAM), de la Universidad Católica de Valencia, dio un nuevo paso con un proyecto internacional para desarrollar un filtro protector capaz de inactivar tanto el SARS-CoV-2 como las bacterias multirresistentes tras un minuto de contacto. El filtro, fabricado con un revestimiento biofuncional de cloruro de benzalconio, también inactiva a las bacterias Staphylococcus aureus y Staphylococcus epidermidis resistentes al antibiótico meticilina. Hay que recordar que las infecciones bacterianas empeoran la neumonía provocada por el coronavirus y suponen una amenaza añadida.
El trabajo ha sido encabezado por Ángel Serrano, acompañado de Miguel Martí y Alberto Tuñón (del mismo grupo), Yukiko Muramoto, Takeshi Noda y Kazu Takayama (Universidad japonesa de Kioto), y Finn Lillelund Aachmann (Universidad Noruega de Ciencia y Tecnología).

Según explica Serrano a DM, “el cloruro de benzalconio es un producto con el que estábamos trabajando desde hace más de un año para otras aplicaciones médicas por su capacidad antimicrobiana. De hecho, en mayo de 2019 realicé una estancia de un mes en la Universidad Noruega de Ciencia y Tecnología y le di este compuesto al profesor Finn Lillelund Aachmann para que lo caracterizara por resonancia magnética”.
Sin embargo, desde el comienzo de la pandemia, “con familiares cercanos trabajando en primera línea que se infectaron, quise contribuir de algún modo a mitigarla. Aunque intenté solicitar un proyecto europeo en colaboración con mis colegas noruegos y una compañía farmacéutica, fue imposible encontrar un laboratorio de bioseguridad disponible que trabajara con el SARS-CoV-2 porque estaban todos saturados haciendo pruebas con fármacos de aplicación inmediata y con el desarrollo de las vacunas”.
Así que cuando se pudo volver al laboratorio después del confinamiento y debido a la imposibilidad de trabajar con el virus real, “empezamos a estudiar un modelo viral que me sugirió Miguel Martí: un virus similar al SARS-CoV-2 que no es infeccioso para los humanos y que podíamos utilizar en nuestro laboratorio de microbiología”.
Tras darle vueltas a posibles aplicaciones no convencionales de este compuesto, “un día hablando con Martí tuve la idea de poner este compuesto en un filtro de mascarilla en forma de recubrimiento micrométrico y ver si era capaz de inactivar ese virus no infeccioso. Realizamos las pruebas y los resultados fueron fulminantes: el filtro tratado eliminaba, en tan sólo un minuto, al cien por cien de los virus”.
Al alcance de todos
Más tarde comprobaron si era capaz también de destruir las bacterias multirresistentes Staphylococcus aureus y Staphylococcus epidermidis, “y también las destruía de forma impresionante”. Con estos resultados contactó con el profesor Kazuo Takayama, de la Universidad de Kioto, que cuenta con un laboratorio de bioseguridad para trabajar con el SARS-CoV-2 para presentarle los resultados. Tras verlos, “dijo de inmediato que le enviara el filtro para probarlo con el SARS-CoV-2”. Al cabo de una semana, habían comprobado que el filtro “también era capaz de desactivar al SARS-CoV-2 en un minuto”.
Dentro de poco, las mascarillas con estos nuevos filtros podrían estar ya en el mercado a un precio muy asequible, pues su método de fabricación es rápido y económico, y el producto clave, el cloruro de benzalconio, no tiene un coste elevado. “El uso correcto de esta tecnología de amplio espectro antimicrobiano es importante para la producción en masa y comercialización de estos filtros para mascarillas, que serán muy útiles para los sanitarios e investigadores que se enfrentan a la pandemia”, apunta Ángel Serrano.
Para facilitar ese trasvase, y en espera de publicar los resultados -ahora están en la plataforma de prepublicación bioRxiv-, “en lugar de buscar un rendimiento económico, descartamos la posibilidad de generar una patente debido a la emergencia sanitaria en la que nos encontramos y consideramos que lo más correcto éticamente era ponerlo en conocimiento lo antes posible de la comunidad científica y las empresas dedicadas a la fabricación masiva de mascarillas”.
Doble protección
Y así, de la escasez inicial se ha pasado en poco tiempo a que un puñado de empresas acelere producción y desarrollos con garantías para una pandemia que no parece calmarse y que ha descubierto la utilidad de esta prenda. Otra empresa española, Protect Line, con sedes en Bilbao, Madrid y Valencia, ha desarrollado una mascarilla dual que protege frente a los bioaerosoles tanto al portador como a los demás, pues reduce la transmisión de agentes infecciosos que el usuario emite a su entorno. Es hipoalergénica y está compuesta en un 43% por tejido sin tejer, en un 30% por tela fundida por soplado y en un 27% por algodón de aire caliente.
Según sus fabricantes, posee una eficacia superior al 94% a la hora de filtrar partículas, superior al 98% en el caso de las bacterias, y tiene una presión de resistencia a las salpicaduras superior a 16 kPa. Cumple todos los requisitos del Reglamento 2016/425 de la Unión Europea (UE) relativo a los equipos EPI y, a su vez, la Directiva 93/42 de la Comunidad Económica Europea relativa a los productos sanitarios. Esta situación convierte a la mascarilla FM0201-966 en una FFP2/IIR, es decir, válida tanto en el ámbito sanitario como fuera de él.
No tan sofisticadas, pero igualmente válidas, son las FFP2 y FFP3 de la firma Star Care. Según Xavier Gastaminza, director general de la empresa, tienen un 98% de eficacia en la filtración de aerosoles de partículas, como las del SARS-CoV-2. Su diseño de 5 capas, hidrófugas, hipoalergénicas y con propiedades electroestáticas, atrae las partículas más pequeñas impidiendo su inhalación. ”La elección correcta de la mascarilla es fundamental para una protección eficaz contra el virus y así, contribuir a una reducción de contagios considerable en esta segunda ola”, aconseja Gastaminza.
Coroscanner : pour quels patients le proposer ? Chez quels patients l’éviter ?
Luc CHRISTIAENS, Cardiologie, CHU de Poitiers
Le coroscanner, ou scanner cardiaque, est une avancée technologique majeure de ces dernières années permettant de visualiser de manière non invasive, le plus souvent en ambulatoire, les structures cardiaques et péricardiques ainsi que le réseau coronaire artériel et veineux. Ceci est devenu possible grâce au développement de détecteurs analysant les structures sur 6 à 12 cm en un seul passage, à des vitesses de rotation du scanner très rapides et à une bonne synchronisation de l’acquisition des images avec l’ECG. Ces avancées ont permis une diminution importante de l’exposition du patient aux rayons X, avec actuellement des coroscanners réalisables pour l’analyse du réseau coronaire pour une dose d’exposition inférieure à 1 mSv.
L’avantage principal du scanner est lié à l’analyse possible a posteriori de toutes les parties d’un volume d’acquisition et à la possibilité d’exclure virtuellement certaines parties pour mieux en analyser d’autres. Ces inconvénients sont marqués principalement par le risque lié à l’exposition aux rayons X et à celui lié à l’injection de produits de contraste iodés. La résolution spatiale est de l’ordre de 0,5 mm, satisfaisante pour l’analyse des structures cardiaques, mais reste un peu limitée pour l’analyse fine des plaques et des sténoses coronaires. La résolution temporelle, 80 à 200 ms, est suffisante pour analyser la cinétique segmentaire, réaliser des mesures de fraction d’éjection ventriculaire droite ou gauche et l’analyse de la mobilité des valves cardiaques.
Sur le plan technique, deux modes d’acquisition des images sont couramment utilisés et le choix de l’un ou de l’autre dépend de l’indication du scanner : • Le mode prospectif avec une acquisition des images uniquement dans une courte période du cycle RR, habituellement 70 % du cycle RR pour l’analyse des artères coronaires. Le mode prospectif peut également être utilisé au cours d’un scanner sans injection de produit de contraste iodé pour le calcul du score calcique coronaire ou score d’Agatston. Du fait de son caractère moins irradiant, c’est le mode le plus utilisé en priorité.
• Le mode rétrospectif consiste en une acquisition continue des images tout au long du cycle RR avec souvent une modulation de dose (baisse des kilovolts) pendant la systole. Ce mode expose le patient à une dose de rayons X 3 à 4 fois supérieure que le mode prospectif, mais permet d’obtenir une visualisation de la cinétique des structures cardiaques. Ce mode est donc intéressant pour une analyse des valves, des prothèses valvulaires cardiaques, des volumes des cavités cardiaques et des fractions d’éjection.
Deux grands types d’indications de coroscanner se dégagent :
• Le coroscanner réalisé pour objectiver la présence ou non de lésions coronaires : coronarographie non invasive.
• Le coroscanner réalisé avant un geste interventionnel structural ou de rythmologie interventionnelle : dans ce cas l’analyse des structures cardiaques est le principal motif de l’examen, on pourrait donc parler de cardioscanner. Dans ce type d’indication, une analyse des artères coronaires sera également réalisée si possible.
Coroscanner et analyse des coronaires : pourquoi ? Pour qui ?
Pour la maladie coronaire, il faut répondre à 3 questions : les artères coronaires sont-elles lésées ? Le myocarde souffre-til ? Quel est le pronostic ?
Les examens à visée morphologique répondent à la première question, les tests fonctionnels ou ischémiques à la deuxième. L’évaluation pronostique est réalisable à partir des deux types de tests, avec la localisation et la multiplicité des sténoses coronaires visualisées, d’une part, et l’importance de l’ischémie myocardique, d’autre part. L’appréciation morphologique, obtenue par coronarographie invasive ou par coroscanner, est la mise en évidence de plaques coronaires éventuellement sténosantes dont la distribution impacte le pronostic du patient. L’aspect fonctionnel est la recherche d’une ischémie myocardique par test d’effort, échographie d’effort ou de stress, scintigraphie ou IRM de stress.
À l’avenir, cet aspect fonctionnel sera probablement évalué également de façon fiable en scanner par le développement de la FFR-CT, évaluation mathématique de la FFR coronaire à partir des données du scanner.
Il est indispensable que les cardiologues s’approprient ces techniques d’imagerie pour rester en première ligne dans la gestion de la maladie coronaire depuis son diagnostic jusqu’à sa prise en charge thérapeutique.
Les deux points forts du coroscanner sont, d’une part, l’évaluation du risque cardiovasculaire à partir du coroscanner non injecté par la mesure du score calcique coronaire et, d’autre part, l’efficacité pour exclure une atteinte coronaire obstructive à partir du coroscanner injecté.
Mesure des scores calciques
La mesure du score calcique coronaire est indiquée en cas de risque coronaire faible à modéré chez des patients asymptomatiques sur le plan angineux (recommandation de classe IIB niveau B)(1) et chez les patients diabétiques asymptomatiques à risque modéré(2). Ce score prend en compte l’étendue des calcifications coronaires et leur densité (figure 1). L’utilisation de ce score permet le reclassement du niveau de risque cardiovasculaire du sujet dans 30 à 40 % des cas. En l’absence de calcification coronaire avec donc un score calcique coronaire égal à zéro, et même en présence de facteurs de risque traditionnels, le risque d’événement cardiovasculaire dans les 5 ans est très faible (< 0,5 % à 50 mois). À l’inverse, un score supérieur à 300 ou au 75e percentile pour l’âge, le sexe et l’ethnie, est considéré comme à haut risque d’événement cardiovasculaire(3). Cette mesure peut être intégrée dans le calcul de probabilité pré-test de sténose coronaire en cas de syndrome coronaire chronique(4).

Figure 1. Coroscanner sans injection. Mesure du score calcique coronaire. En blanc : calcifications coronaires et aortiques. Images de droite : repérage en vert des calcifications du réseau coronaire gauche proximal. Images de gauche : repérage en vert des calcifications du réseau coronaire droit segment 3.
La même technique est utilisée couramment pour mesurer le score calcique de la valve aortique en cas de rétrécissement aortique. Chez l’homme, le rétrécissement aortique est très probablement serré si le score calcique valvulaire aortique est ≥ 3 000, probablement serré si ≥ 2000, et probablement non serré si < 1 600. Pour les femmes, ces valeurs seuils sont respectivement ≥ 1 600, ≥ 1 200 et < 800. Ces valeurs sont utiles en cas de surface valvulaire aortique < 1 cm² avec un gradient moyen < 40 mmHg et une fraction d’éjection ventriculaire gauche préservée(5).
Les calcifications péricardiques sont également bien quantifiées en coroscanner avec ou sans injection de produit de contraste iodé avec synchronisation cardiaque (figure 2).
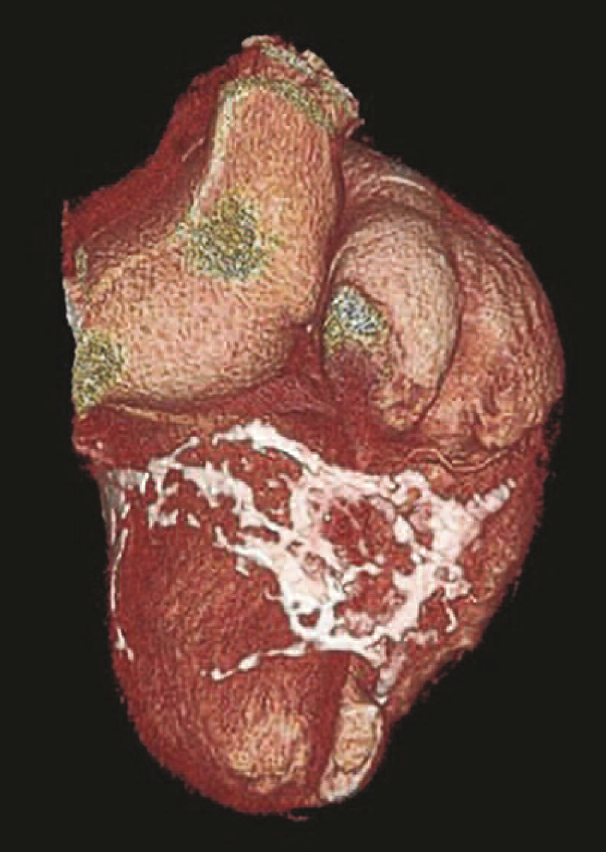
Figure 2. Calcifications péricardiques étendues visualisées en coroscanner.
Coroscanner avec injection de produit de contraste iodé (coronarographie non invasive)
Cet examen ne peut être réalisé qu’après s’être assuré de l’absence d’allergie aux produits de contraste iodé et d’insuffisance rénale sévère. Il nécessite une voie veineuse périphérique de bonne qualité. Il est fréquent d’utiliser une injection intraveineuse de bêtabloquant associé à un dérivé nitré en spray pour obtenir une qualité d’image optimale. Le risque lié à l’exposition aux rayons X doit toujours être considéré, d’autant plus chez la femme jeune en raison de l’exposition mammaire, même si le développement des machines et des pratiques permet une dose d’exposition en routine de l’ordre de 1 à 3 mSv et régulièrement de moins de 1 mSv dans les équipes expérimentées avec un matériel de dernière génération. Un dosage de bêta-HCG est réalisé avant le scanner chez les femmes en âge de procréer. L’obésité morbide et les rythmes cardiaques très irréguliers restent un obstacle. Les extrasystoles isolées, les rythmes électro-entraînés et la fibrillation atriale avec une fréquence ventriculaire entre 40 et 80 par minute ne sont plus des contre-indications au coroscanner à visée coronaire et encore moins pour une analyse des structures cardiaques avant intervention de type TAVI, occlusion d’auricule gauche ou ablation de fibrillation atriale.
Le coroscanner est une excellente technique pour réaliser une étude anatomique des artères coronaires de manière quasi non invasive et en ambulatoire au cours d’un examen qui dure environ 15 minutes. L’acquisition des images en elle-même est très brève au cours d’une apnée et d’un à deux cycles cardiaques. Sa valeur prédictive négative pour les sténoses coronaires est très élevée, supérieure à 95 %. C’est donc un examen fiable pour s’assurer de l’absence de lésion coronaire. Ses indications sont donc logiquement les patients symptomatiques à probabilité faible à intermédiaire de syndrome coronaire chronique (classe IB), les patients avec une discordance entre la clinique et le résultat de tests ischémiques ou des tests ischémiques non concluants (classe IIa), le patient diabétique asymptomatique (classe IIB), et dans le bilan préopératoire de valvulopathie (classe IIa)(2,4,5). L’utilisation du scanner dans le bilan initial d’une suspicion de coronaropathie stable a fait la preuve de son efficacité par rapport à une prise en charge traditionnelle, avec une réduction significative du nombre de décès et d’infarctus du myocarde non fatal avec un suivi moyen de 4,8 ans dans l’étude Scot-Heart(6).
Dans la situation de syndrome coronaire aigu à faible risque (pas de modification notable de l’ECG et de la troponine, stabilité clinique et rythmique), le coroscanner a une indication de classe IIa. Dans cette situation, il faut rechercher attentivement la présence de plaque coronaire non calcifiée pouvant être responsable d’une sténose coronaire significative.
En cas de calcifications coronaires visualisées avant l’injection de produit de contraste, cette injection pourra être abandonnée au profit de la réalisation de test ischémique si ceuxci n’ont pas été déjà réalisés ou d’une coronarographie si l’ischémie apparaît probable.
Le coroscanner garde malgré les progrès technologiques une spécificité médiocre pour l’appréciation du degré de sténose, notamment en cas de plaque calcifiée. C’est la raison pour laquelle le coroscanner est un mauvais outil pour surveiller une maladie coronaire déjà connue en dehors de cas spécifiques tels que le contrôle d’un stent de diamètre ≥ 3 mm sans autre lésion coronaire associée ou l’analyse de pontages coronaires. La recherche d’une resténose intrastent est souvent possible quand le diamètre du stent est ≥ 3 mm, mais le reste du réseau coronaire peut être d’évaluation difficile ou non fiable en cas de lésions coronaires multiples associées.
Malgré cette faiblesse dans l’appréciation du degré de sténose, un des avantages du coroscanner par rapport à la coronarographie est l’appréciation possible des plaques à l’origine des sténoses coronaires : localisation, volume des plaques et aspect calcifié, mixte ou hypodense (figure 3). Il est actuellement habituel de recourir à la classification CAD RADS pour stratifier l’atteinte coronaire d’un patient à partir de la localisation et de l’aspect des plaques coronaires associés à leur degré de sténose, et orienter sa prise en charge thérapeutique(7). Le risque d’événement coronaire majeur est proportionnel à la classe CAD RADS.
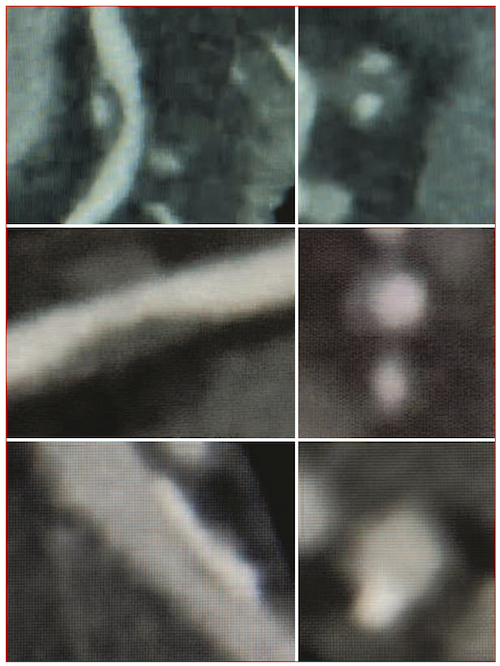
Figure 3. Types de plaque coronaire en coroscanner injecté. Vue longitudinale en mode MIP à gauche avec correspondance en petit axe à droite. De bas en haut : plaque mixte, plaque non calcifiée et plaque calcifiée.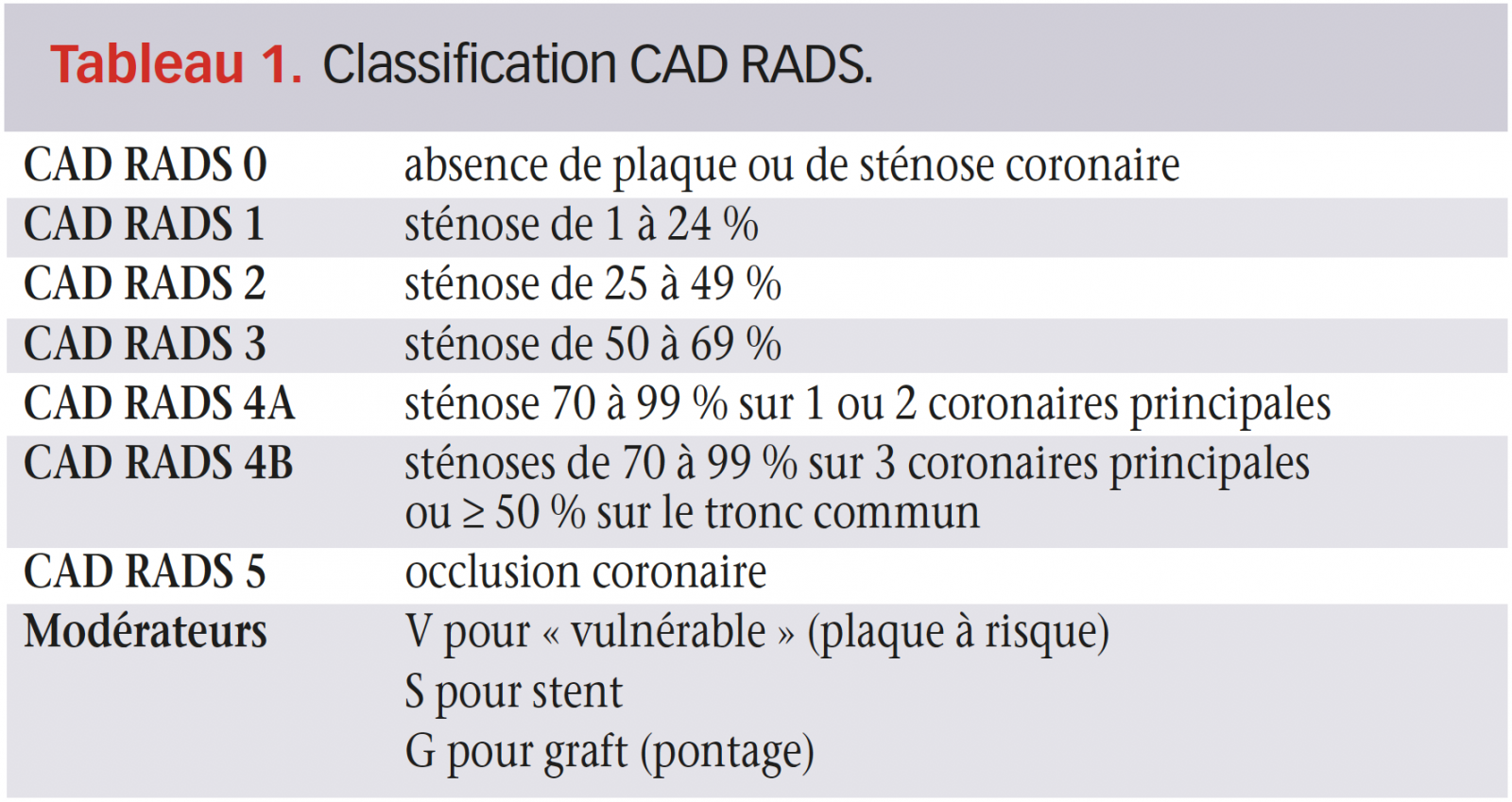
Le coroscanner est également très efficace dans les anomalies de naissance des artères coronaires en permettant une analyse précise de l’ostium coronaire, de son angle de raccordement par rapport à l’aorte, de son éventuel trajet inter-aortico-pulmonaire (figure 4). Il en est de même pour l’analyse des fistules coronaires et la localisation des pontages coronaires, notamment en l’absence de compte rendu opératoire ou avant une chirurgie redux (figure 5).
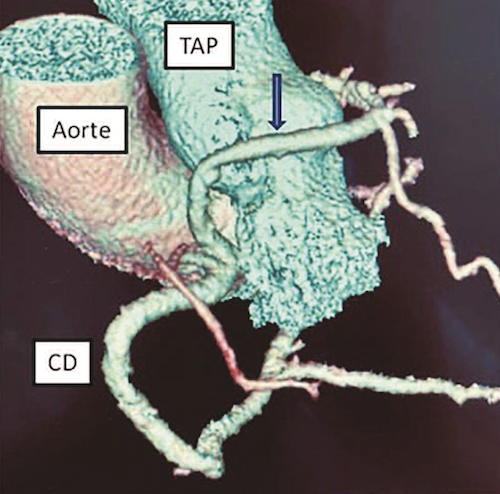

Figure 4. Anomalie de naissance de coronaire avec une coronaire unique naissant de l’ostium coronaire droit, la branche coronaire gauche passant en avant du tronc de l’artère pulmonaire.
Figure 5. Pontage artère thoracique interne gauche pédiculé anastomosé à l’interventriculaire antérieure (IVA). À gauche : vue en mode VRT. À droite : vue en mode MIP. Flèche : clip d’hémostase.
Risque CV : risque cardiovasculaire ; SCC : syndrome coronaire chronique ; SCA : syndrome coronaire aigu ; IMC : indice de masse corporelle ; TAVI : transartériel valve implantation ; FA : fibrillation atriale.
Coroscanner et cardiologie interventionnelle structurale
Le coroscanner est actuellement incontournable pour définir la stratégie de réalisation d’un TAVI : mesure de la surface de l’anneau valvulaire aortique qui servira à déterminer la taille et le type de la bioprothèse à utiliser (figure 6), évaluer la voie d’abord artérielle fémorale ou autre, mesurer la hauteur d’implantation des artères coronaires, déterminer l’incidence de travail et prévoir les éventuelles complications. Pendant la procédure, la technique de fusion des images de scanner et de scopie peut être utile pour limiter la quantité de produits de contraste (figure 7). En postprocédure, le scanner permettra d’apprécier si nécessaire le déploiement de la bioprothèse, la mobilité des feuillets de la bioprothèse et la recherche de thrombus non ou peu obstructif (figure 8 et 9).

Figure 6. Mesure de la surface de l’anneau valvulaire aortique en scanner avant une procédure de TAVI.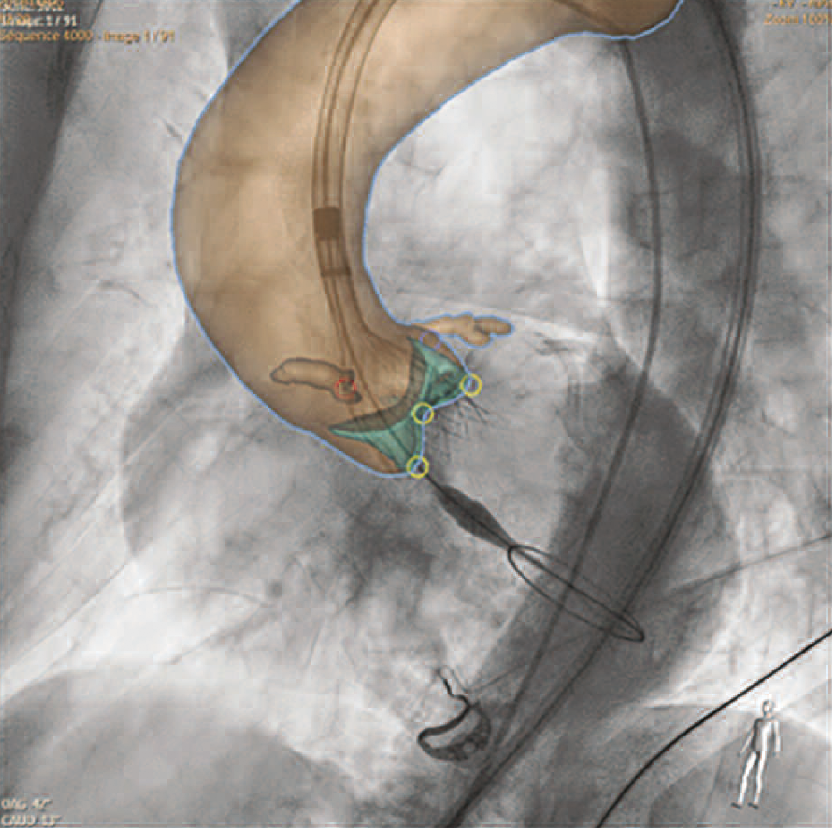
Figure 7. Fusion des images de scopie et de scanner per-procédure TAVI (mise en place d’une CoreValve™).

Figure 8. Contrôle par scanner après TAVI : défaut de déploiement d’une bioprothèse aortique CoreValve™ sur un amas calcaire valvulaire. Défaut visualisé (B, C, D) ou non (A) suivant l’incidence de vue.
Figure 9. Contrôle par scanner après TAVI : thrombus incomplètement obstructif (flèche) d’une bioprothèse Edwards™.
La reconstruction 3D de structures complexes comme l’auricule gauche est facile en scanner et une reproduction fiable par imprimante 3D peut être réalisée, permettant dans les cas complexes d’essayer différents types de prothèses d’occlusion d’auricule gauche ex vivo. Même en l’absence de reconstruction 3D, le choix du type et de la taille de la prothèse pourra être fait à partir des images de scanner. Le coroscanner est un outil aussi performant que l’ETO pour détecter la présence d’un thrombus dans l’auricule gauche, qualité indispensable avant d’envisager une occlusion de l’auricule gauche ou une ablation de fibrillation atriale. L’analyse en coroscanner des calcifications de l’anneau mitral et de la géométrie du ventricule gauche est très utile avant d’envisager la pose d’une bioprothèse mitrale percutanée.
Coroscanner et rythmologie
Le coroscanner avec injection de produit de contraste iodé et nouvelle acquisition des images à un temps tardif est au moins aussi efficace que l’ETO pour détecter la présence de thrombus dans l’auricule gauche.
En plus de cette visibilité de l’auricule gauche, le coroscanner permet une bonne analyse de l’abouchement et de la distribution des veines pulmonaires ce qui en fait un outil très utile avant une ablation de fibrillation atriale. La reconstruction 3D du volume de l’oreillette gauche pourra être couplée à la cartographie électrique « peropératoire » pour localiser avec précision les tirs de radiofréquence. L’appréciation des rares sténoses de veine pulmonaire consécutives aux procédures d’ablation pourra être effectuée en coroscanner. Le coroscanner réalisé avant ablation de fibrillation atriale permettra par la même occasion de statuer sur le réseau coronaire du patient. La cartographie veineuse coronaire obtenue au cours d’un scanner cœur standard peut se révéler utile pour optimiser une procédure de resynchronisation ventriculaire.
Conclusion
Le coroscanner est un outil indispensable dans la panoplie du cardiologue moderne, à la fois pour l’évaluation du pronostic cardiovasculaire du patient, pour la compréhension de la maladie coronaire, la confirmation très souvent nécessaire de l’absence de lésions coronaires significatives chez un patient et un grand nombre de procédures de cardiolo gie interventionnelle structurales ou de rythmologie interventionnelle.
Références
Cliquez sur les références et accédez aux Abstracts sur 
1. Mach F et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk: The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis S Rechercher l’abstract
2. Cosentino F et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: The Task Force for diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) a Rechercher l’abstract
3. Sarwar A et al. Diagnostic and pronostic value of absence of coronary artery calcification. J Am Coll Cardiol Img 2009 ; 2 : 675-88. Rechercher l’abstract
4. Knuuti J et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. The Task Force for the diagnosis and management of chronic coronary syndromes of the European Society of Cardiology (ESC). Eur Heart J 2020 ; 41 : 407-7 Rechercher l’abstract
5. Baumgartner H et al. 2017 ESC/ EACTS Guidelines for the management of valvular heart disease. Eur Heart J 2017 ; 38 : 2739-91. Rechercher l’abstract
6. The SCOT-HEART Investigators. Coronary CT angiography and 5-year risk of myocardial infarction. N Engl J Med 2018 ; 379 : 924-33. Rechercher l’abstract
7. Xie J et al. The coronary artery disease- reporting and data system (CADRADS). Prognostic and clinical implications associated with standardized coronary computed tomography angiography reporting. J Am Coll Cardiol Img 2018 ; 11 : 78-89. Rechercher l’abstract
Retinógrafo portátil permite diagnosticar doenças oculares à distância

Um aparelho portátil ligado a um smartphone produz imagens precisas da retina, permitindo detectar doenças do fundo do olho a um custo bem mais baixo do que os métodos convencionais.
Criado pela Phelcom Technologies, o Eyer é o primeiro retinógrafo portátil com qualidade de equipamento de mesa. O equipamento consegue possibilitar o diagnóstico por telemedicina, um benefício a mais em tempos de pandemia.
Usando a tecnologia que já existe e equipamentos que a maioria das pessoas já possui em casa, a telemedicina pode gerar diagnósticos e tratamentos mais rápidos, aumentando a eficiência nos atendimentos, reduzindo o estresse do paciente e a grande demanda de pessoas, no sistema público de saúde.
“No caso de doenças oftalmológicas, alguns diagnósticos podem ser realizados através do Eyer, um aparelho de alta tecnologia, integrado ao smartphone, que permite a realização de exames, automaticamente sincronizados com a internet, habilitando diagnósticos remotos”, explica Caio Regatieri, oftalmologista e sócio-proprietário da Videomedic, software de gestão e atendimento médico em planos de saúde.
Funções inteligentes
O Eyer possui funções inteligentes que auxiliam o diagnóstico médico, capturando a foto do fundo de olho, com alto nível de detalhes, facilitando o compartilhamento e o acesso aos dados dos exames, na nuvem. É possível realizar exames de retina, sem a necessidade de dilatação da pupila, em qualquer lugar do mundo, com conforto e rapidez.
Na frente da câmera do celular, fica um conjunto óptico projetado para iluminação e imageamento da retina. Quando as imagens são produzidas, o aplicativo que opera o aparelho as envia pela internet para um sistema web, chamado de Eyer Cloud, que permite armazenar e gerenciar os exames dos pacientes.
Caso não haja acesso a Wi-Fi ou rede 3G ou 4G no momento do exame, as imagens ficam salvas no aparelho e são enviadas para a nuvem assim que houver conexão com a internet.
“Qualquer profissional da saúde, desde que seja treinado, poderá realizar exames de retina de alta qualidade, em menos de um minuto. Em uma Unidade de Pronto Atendimento (UPA), por exemplo, que não tenha a especialidade de oftalmologia, a própria enfermagem ou o clínico médico poderá realizar o exame e enviar para outra unidade, que tenha a especialidade. O diagnóstico é realizado à distância e o problema é resolvido rapidamente. Se for algo mais grave, o paciente já será encaminhado ao especialista, imediatamente”, esclarece Caio Regatieri.
Produção e custos
O Phelcom Eyer alcançou a marca de 100 mil exames realizados. O equipamento foi lançado no mercado há apenas um ano e quatro meses.
O dispositivo já sai da fábrica acoplado a um smartphone de última geração e custa cerca de US$ 5 mil. O aparelho convencional mais usado atualmente precisa ser ligado a um computador e custa em média R$ 120 mil.
Os exames de segmento anterior e retinografia colorida são os mais realizados atualmente. “Cerca de 850 profissionais utilizam a tecnologia e há aproximadamente 90 mil pacientes cadastrados na nossa plataforma on-line, o Eyer Cloud”, conta José Augusto Stuchi, cofundador e CEO da Phelcom, José Augusto Stuchi.
A expectativa é produzir 200 mil exames até metade de 2021.
*Esse artigo foi revisado pela equipe médica da PEBMED
Referências bibliográficas:
A tomossíntese das mamas é melhor que a mamografia digital?

Um novo estudo prospectivo procurou avaliar a acurácia diagnóstica para o rastreamento de câncer de mama em estádios iniciais com a tomossíntese das mamas (T), também chamada de “mamografia em 3D” pelas inúmeras imagens em diferentes ângulos que esta técnica proporciona, quando comparada à mamografia digital (MD), já que pouco sabemos sobre o valor do rastreamento subsequente de uma população com a T.
Método do estudo
Foram incluídas de forma prospectiva 34 mil mulheres na região de Verona (IT) entre 04/2015 e 03/2017 e quase 33 mil destas foram avaliadas novamente entre 04/2017 e 03/2019, metade com MD metade com T. A mediana de idade foi de 58 anos. Foi avaliada a performance do rastreamento através da taxa de detecção de câncer (TDC) e da taxa de reconvocação (TR) –recall. O grupo controle desta pesquisa foi um grupo de 28 mil mulheres que fizeram o rastreamento com mamografia digital realizada entre 2013 e 2014. Foram comparados os estadiamentos dos casos de câncer nestas diferentes formas de rastreamento.
A TDC foi maior para o grupo da T do que MD (9,3 vs 5,3% por 1000 mulheres rastreadas e no segundo teste 8,1 vs 4,5%). A TR foi semelhante entre os 2 grupos. A repetição do rastreamento mostra que a proporção de pacientes diagnosticadas no estádio II foi de 14,5% – 19 de 131 casos no grupo T contra 27% (30 de 110 casos) no grupo controle que rastreou com MD. Outro dado importante: o valor preditivo positivo do recall foi bem maior no grupo T (23,8 vs 12%).
A conclusão dos autores é que a repetição do rastreamento com T detectou mais cânceres de mama do que a MD e achou menos casos de câncer no estádio II e estádios ainda maiores.
Nos EUA, a tomossíntese das mamas está aprovada desde 2011 e dados de Outubro deste ano mostram que 42% dos exames lá já são de T.
Uma das novidades deste estudo é o desempenho em um segundo “round” subsequente, já que a maioria dos estudos anteriores avaliava apenas o primeiro “round” comparando T com MD. É preciso avaliar se essa melhoria de rendimento se mantém não só nos primeiros “rounds”, mas num tempo maior de seguimento.
De qualquer maneira, lá nos EUA a pressão das indústrias de equipamentos e outros fatores estão fazendo a migração de uma tecnologia para a outra, ainda que nem todas as evidências estejam maduras para esta transição.
Uma das preocupações com a possível maior dose de radiação com a T não procede, pois a diferença atual entre uma MD completa convencional e uma T é pequena em especial se o exame for repetido em intervalos habituais (1-2 anos).
Limitações
O estudo, no entanto, tem limitações, já que não foi randomizado, foi uni-institucional e usou apenas equipamento de T de um único fabricante. Não temos informações sobre possíveis diagnósticos de câncer de intervalo. Alguns podem criticar que detectar mais cânceres por T não seria muita vantagem, já que em tese poderíamos ter mais casos de ótimo prognóstico como luminais A, in situ, levantando a questão do overdiagnosis, mas ao detectar menos casos também de cânceres de estádio II ou mais avançados, a T cumpre sua “missão” de fazer detecção ainda mais precoce que a MD e evitar diagnósticos muito avançados que no “round” seguinte seriam diagnosticados ainda mais tardiamente.
No Brasil, a cobertura da tomossíntese das mamas não é obrigatória e o reembolso ainda é exceção de uma minoria das operadoras da saúde suplementar. O custo do exame em si não é muito mais caro do que de uma MD em uma clínica particular, mas o aparelho tem um custo muitas vezes superior ao de um bom mamógrafo digital, estando disponível ainda em número limitado de clínicas e hospitais. A tecnologia avança, o custo pode cair, o reembolso pode ser ampliado, mas ainda temos muitas dúvidas científicas no uso “indiscriminado” como ferramenta diagnóstica para rastreamento e detecção precoce do câncer de mama.
Tomossíntese é melhor que mamografia digital? Parece que sim. Em mulheres um pouco mais jovens, mamas densas, etc? Parece que sim. Qual a maior limitação? O custo do aparelho, reembolso, disponibilidade. Na saúde suplementar está caminhando lentamente em nosso país, mas está.
E na saúde pública? A questão é muito mais complexa, precisamos lutar para aumentar a nossa cobertura mamográfica pífia de cerca de 20% (ante 70% recomendados pela OMS) na população alvo do ministério, 50-69 anos. Ainda falta muito para brigar por T no SUS. Temos que reduzir os casos inoperáveis, reduzir fila intermináveis, diagnosticar e tratar mais rapidamente. O SUS tem coisas muito mais urgentes na agenda.
Autor(a):
Gilberto Amorim
Formado em 1992 na UFRJ • Residência Médica em Clínica Médica no HUCFF – UFRJ • Residência em Oncologia Clínica no INCA • Oncologista do INCA de 01/1998 até 04/2008 –Chefe do Serviço do HCIII de 11/1999 até 05/2001 e de 12/2003 até 12/2005 • Membro Titular da SBOC desde 1996 • Membro titular da “ASCO” desde 2001 e da “ESMO desde 2016 • Sócio Honorário da Sociedade Brasileira de Mastologia desde 2009 • Oncologista e Coordenador Nacional de Oncologia Mamária da “Oncologia D’Or”, desde 05/2011 • Membro voluntário do Comitê Científico da FEMAMA, do INSTITUTO ONCOGUIA e da Fundação Laço Rosa
Referências bibliográficas:
- Caumo F, Montemezzi, Romanucci G et al. Repeat Screening Outcomes with Digital Breast Tomosynthesis Plus Synthetic Mammography for Breast Cancer Detection: Results from the Prospective Verona Pilot Study; Radiology 2020; 00:1–9. doi: 10.1148/radiol.2020201246.
Confirmar un test de embarazo: cada vez más seguro con test fiables
Esperar a que aparezca una línea de color para confirmar un embarazo pasó a la historia. Los nuevos test indican incluso la semana de gestación.

Para saber si una mujer está embarazada o no, la clave fundamental se encuentra en la hormona gonadotropina coriónica humana (hCG). Durante el embarazo, primero el óvulo fecundado y luego la placenta producen la hCG. El óvulo fecundado suele implantarse en el revestimiento del útero o endometrio entre 6 y 8 días antes de la ausencia del periodo, momento en el cual aparecen pequeñas cantidades de hCG en la sangre y en la orina de la madre. Aunque los niveles de hCG son muy bajos al principio, van aumentando con gran rapidez y de forma predecible durante las primeras semanas del embarazo.
Y para conocer si esta hormona está presente, se puede analizar la sangre o la orina. En el primer caso, se trata de un análisis que se llevan a cabo en laboratorio y que analiza la cantidad de esta hormona presente en la extracción de sangre. El segundo consiste en una prueba de autodiagnóstico disponible en oficina de farmacia y el análisis es cualitativo.
“La fiabilidad de las pruebas de autodiagnóstico depende un poco del test, pero suelen ser muy fiables si se realizan en el momento correcto, es decir, cuando la concentración de hCG es superior al umbral de detección del test. En estos casos, tienen hasta un 99 % de fiabilidad. En los últimos años, algunos test de orina han mejorado en cuanto a sensibilidad, llegando a detectar cantidades muy pequeñas de la hormona”, explica María Romero, farmacéutica del Centro de Información del Medicamento (CIM) del Colegio de Farmacéuticos de Sevilla.
Hay investigaciones para mejorar el diseño y los materiales de los test de embarazo para que sean biodegradables
Francisca Maria Santandreu, coordinadora de Formación y del CIM del Colegio de Farmacéuticos de las Islas Baleares, coincide en señalar esta alta fiabilidad, “siempre que se sigan las instrucciones del fabricante y se usen correctamente”. Asimismo, señala que hoy en día en el mercado se pueden encontrar una gran variedad de pruebas de embarazo, atendiendo a la sensibilidad y a la cantidad de hCG que son capaces de detectar en la orina de la mujer.
De esta forma, las diferentes pruebas de embarazo se pueden clasificar en cuatro categorías:
- Ultrasensibles: cuando detectan una concentración de hormona desde 5 mlU/mL; de alta sensibilidad, cuando es de 10 a 15 mlU/mL.
- Sensibles: si lo hace de 20 a 25 mlU/mL.
- Estándar: si es de 25 a 50 mlU/mL.
“Cuanta más sensibilidad tengan, antes detectarán la hCG en orina y se podrían realizar unos días antes del día que se espera que se inicie el período”, añade Santandreu.
Según la experta, existen investigaciones para la mejora del diseño y de los materiales, por ejemplo, para hacerlos biodegradables y más respetuosos con el planeta. “En los test más clásicos el resultado aparece como una línea de color. Ahora existen versiones digitales donde el resultado se muestra con la palabra embarazada o no embarazada, e incluso, según el test, se especifican las semanas de gestación”, continúa.
También comenta que “las pruebas en orina resultan fiables y menos invasivas que la extracción de sangre. La exactitud la evalúa cada fabricante mediante estudios comparativos con métodos de referencia. Varía según la empresa, pero podemos decir que tanto la sensibilidad, la especificidad como la precisión de estas pruebas es igual o mayor al 99%. Sin embargo, en los casos en los que existan dudas, la mejor forma de comprobar un embarazo es realizar un análisis de sangre por punción venosa previa valoración médica”.
Funcionamiento sencillo
Los test que existen de autodiagnóstico tienen todos una forma de funcionamiento sencilla. Es necesario poner en contacto la orina de la mujer con una banda o tira química, que permite después de unos minutos obtener el resultado. “Existe la creencia de que el test debe realizarse con la primera orina de la mañana, pero, en realidad, puede hacerse en cualquier momento del día”, comenta Romero.
Francisca Mª Santandreu (farmacéutica): “Las pruebas de orina resultan fiables y menos invasivas que los análisis de sangre”
Ahora bien, la portavoz del COF de las Islas Baleares lo que aconseja es que, “aunque los test de embarazo pueden realizarse a cualquier hora del día, a primera hora de la mañana es cuando la orina está más concentrada y es entonces cuando es más recomendable hacerlo”.
Antes de comenzar la prueba hay que lavarse bien las manos y retirar el dispositivo de su envoltorio y se indica recoger la orina en un envase estéril. “Se puede sospechar de un embarazo desde la primera falta, es decir, la fecha prevista de la menstruación”, comenta Romero, una apreciación en la que coincide su colega de profesión.
Falsos positivos y negativos
Aunque se ha trabajado mucho para mejorar la fiabilidad de las pruebas de embarazo, no están libres de poder errar, aunque es muy difícil que esto se pueda producir. “Es muy poco probable que se produzca un falso positivo, puesto que los test son muy específicos para la detección de hCG. No obstante, hay algunos casos en los que puede aparecer esta hormona en la orina sin que la mujer esté embarazada, por ejemplo, si están utilizando medicamentos para la fertilidad que contengan esta sustancia, en algunos tipos de cáncer o si ha estado embarazada recientemente, incluyendo aquellos casos de embriones que no se han llegado a implantar”, apunta Romero. Santandreu añade también otras posibles causas para un falso positivo, entre ellas, algunas patologías, como quistes ováricos y trastornos hormonales.
Debido a que la concentración de hCG en orina aumenta con el tiempo, si el test se realiza antes de que sea detectable es posible que dé como resultado un falso negativo. “También se puede dar un falso negativo si la orina no tenía la concentración de hCG suficientemente alta, por ejemplo, porque es una orina muy diluida por beber demasiado líquido antes de realizarse el test”, comenta Santandreu.
Una prueba de embarazo será menos precisa si está vencida o si se utiliza de una forma inadecuada. Por eso, es importante también revisar la fecha de vencimiento y leer cuidadosamente las instrucciones que vienen con la prueba. Con todo esto presente, las expertas señalan cómo los test positivos indican casi con total seguridad que existe un embarazo.
En los casos en que la prueba dio como resultado negativo y después de haberlo repetido por segunda vez, la menstruación continúa sin llegar, lo ideal será acudir a una consulta con el ginecólogo para verificar la causa del problema e iniciar el tratamiento adecuado, en caso de ser necesario. “Los test negativos deben repetirse a los pocos días si persiste la falta de menstruación o acudir a un centro sanitario para que realicen una prueba en sangre y confirmar de esta manera el resultado”, añade María Romero.
“En cuanto la paciente tenga un resultado positivo de un test de embarazo, debería contactar con Atención Primaria para la derivación al especialista y la realización de pruebas complementarias, como son analíticas y ecografías. Su matrona revisará, entonces, la historia clínica, valorará el riesgo del embarazo y le hará las primeras recomendaciones”, explica la farmacéutica de Baleares.
De todas las pruebas de embarazo que se pueden realizar en casa, el más fidedigno es el que se compra en la farmacia. Esto no impide que existan algunos otros métodos que, sin embargo, no deberían considerarse una forma fiable para confirmar o descartar un posible embarazo.
Así, por ejemplo, cada vez son más comunes las pruebas on line, que deben considerarse más una forma de saber cuál es el riesgo de estar embarazada, no debiendo servir como test definitivo ni sustituir la prueba de farmacia o de laboratorio. Estas pruebas on line se basan en los síntomas genéricos del embarazo, así como actividades de riesgo, pero no son capaces de evaluar a cada mujer de manera individual ni tomar en cuenta factores más específicos.
También existen diferentes creencias relacionadas con la lejía, que se supone que es capaz de reaccionar con la hCG produciendo espuma; hervir la orina, que se basa en la teoría de que al hervir proteínas, como ocurren en el caso de la leche, se produce espuma y la hCG es un tipo de proteína, o la prueba del vinagre, basada en el concepto de que el pH de la orina en el embarazo suele ser menos ácido que el de una mujer no embarazada.
Ninguna de ellas tiene evidencia de que funcione y algunas incluso pueden suponer un riesgo para la salud, como la prueba de introducir un bastoncillo para identificar precozmente si el periodo está bajando y que puede causar lesiones o aumentar el riesgo de contraer una infección.
Todo empezó en Egipto
La ausencia de la menstruación en la mujer es uno de los primeros síntomas que pueden evidenciar que se ha quedado embarazada. Sin embargo, los retrasos en los ciclos de ovulación no son extraños, además de existir otras causas que pueden ocasionar la pérdida de la regla. Por eso, los test de embarazo puede convertirse en una herramienta importante para salir de dudas y poder tomar decisiones.
La prueba de embarazo más antigua registrada se halla narrada en un papiro del Antiguo Egipto, que se encuentra en el Museo Egipcio, de Berlín. Para detectar el embarazo se hacía orinar a la mujer durante varios días sobre semillas de trigo y cebada. Si germinaba la cebada, el hijo sería varón. Si germinaba el trigo, sería mujer. En caso de no germinar ninguna semilla, no había embarazo.
En la década de los años 30 en Sudáfrica, Lancelot Hogben, Harry Zwarenstein y Hillel Shapiro desarrollaron lo que se conoció como la prueba de la rana, un test que se usó intensivamente hasta los años 60 y que consiste en inyectar a una rana o sapo hembra la orina de la paciente. Esta orina, que en caso de que la mujer esté embarazada contiene hormona gonadotropina coriónica humana o GCH, estimulaba la ovulación del animal. Si la rana desovaba en 24 horas el test se consideraba positivo.
En 1947, Galli Mainini descubrió la prueba del sapo, con la que se obtenían los resultados mucho antes y que consistía en inyectar la orina de la mujer en un sapo. Si a las tres horas el animal eyaculaba, se confirmaba el embarazo.
En la actualidad, los test de embarazo que se pueden encontrar en las oficinas de farmacia siguen utilizando la orina como base, algo que no ha cambiado desde el Antiguo Egipto. Sin embargo, su fiabilidad sí que ha mejorado de forma sustancial desde entonces, así como la facilidad para realizar el test y la rapidez para conocer el resultado.
Coronavirus : une appli serait capable de repérer l’infection en analysant la toux

Etats-Unis — Une équipe de chercheurs du Massachusetts Institute of Technology (MIT) a développé une appli mobile qui serait capable de repérer les patients infectés par le SARS-CoV-2 grâce aux caractéristiques audio de leur toux.
Toux forcée
Le repérage des personnes infectées par le SARS-CoV-2 reste difficile lorsqu’elles sont asymptomatiques. La politique consistant à tester tout un chacun régulièrement ne semblant pas d’actualité…
Un problème sans solution ? Pas si l’on en croit une équipe de chercheurs du MIT. D’après Jordi Laguarta et ses collègues, la solution pourrait venir de l’intelligence artificielle (IA).
L’application qu’ils ont mise au point serait capable de dire si oui ou non la toux d’une personne est caractéristique de l’infection au SARS-CoV-2. Pour cela, il suffit que la personne se force à tousser et enregistre sa toux via l’appareil sur lequel il a téléchargé l’application (smartphone, ordinateur, tablette…)
L’analyse algorithmique qui s’ensuit déboucherait sur un diagnostic affichant une sensibilité de 98,5 % et une spécificité de 94,2 %, d’après l’article publié par la revue IEEE Open Journal of Engineering in Medicine and Biology.
« La mise en œuvre de cet outil pourrait réduire la propagation de la pandémie si tout le monde l’utilisait avant d’entrer dans une salle de classe, une usine ou un restaurant », affirme le co-auteur Brian Subirana dans un communiqué de presse.
70 000 échantillons
Avant même la survenue de la pandémie, plusieurs équipes de chercheurs avaient mis au point des algorithmes permettant de détecter des maladies comme la pneumonie ou l’asthme au moyen d’une toux forcée.https://9be9ac0bc012c21ab2621349722f4d22.safeframe.googlesyndication.com/safeframe/1-0-37/html/container.html
L’équipe du MIT a élaboré des modèles mathématiques visant à identifier spécifiquement les patients atteints de maladie d’Alzheimer sur base de leur toux. Cette forme de démence affecte notamment les cordes vocales, au travers de modifications neuromusculaires.
Jordi Laguarta et ses collaborateurs ont utilisé ces données pour vérifier si l’IA pourrait détecter les anomalies de la toux et suggérer également d’autres diagnostics.
En avril, ils ont entrepris de recueillir des données sur la toux forcée, tant auprès de volontaires en bonne santé que de patients infectés par le SARS-CoV-2. Tous les participants à l’étude ont enregistré leur toux via un smartphone, une tablette ou un ordinateur et ont envoyé leurs fichiers audio vers un site web dédié. Ils ont également rempli un questionnaire portant sur leur symptomatologie éventuelle, qu’ils aient ou non subi un test de dépistage du SARS-CoV-2. À ce jour, les chercheurs ont recueilli des données portant sur plus de 70.000 échantillons.
Sensibilité et spécificité élevées
Dans un premier temps, les chercheurs ont vérifié s’il était possible de différencier les patients au moyen de biomarqueurs acoustiques. Ils y sont effectivement arrivés en se basant sur l’algorithme élaboré pour la maladie d’Alzheimer.
Les auteurs attribuent cette capacité discriminante à des modifications marginales qu’entraine l’infection par le SARS-CoV-2 au niveau des voies respiratoires, des poumons et – surtout – des muscles en jeu.
L’outil a été ensuite alimenté par 4.256 fichiers audio provenant de volontaires en bonne santé et de patients infectés. 1.054 autres enregistrements ont été introduits dans l’algorithme pour déterminer dans quelle mesure les patients Covid-19 asymptomatiques peuvent être identifiés par leur toux forcée.
Lors de la validation chez les personnes ayant déclaré leur résultat de test SARS-CoV-2, le modèle a affiché une sensibilité de 98,5 % et une spécificité de 94,2 %. En examinant uniquement le sous-groupe de patients asymptomatiques, les chercheurs ont calculé une sensibilité de 100 % et une spécificité de 83,2 %.
Vers une appli gratuite
Les auteurs affirment que leur outil n’est pas destiné à diagnostiquer la maladie chez un patient symptomatique. Son intérêt réside plutôt dans la reconnaissance des patients asymptomatiques, pour les diriger ensuite vers un médecin.
L’équipe du MIT travaille actuellement avec une entreprise sur le développement concret d’une application gratuite et basée sur leur modèle.
Des échantillons audio supplémentaires seront également recueillis dans les hôpitaux.
L’objectif final, en installant une telle application dans les appareils munis de micros et en offrant une analyse en ligne, est de permettre à chaque personne de recevoir automatiquement – et idéalement au quotidien – une évaluation de son statut infectieux. En théorie, cette application pourrait fonctionner continuellement, en arrière-plan.
L’étude comporte cependant quelques faiblesses. L’une d’entre elles tient dans le fait que les personnes testées déclaraient elles-mêmes le statut de leur test Covid, et que ces informations n’étaient pas (toujours) vérifiables.
Jori Laguarta, Brian Sulinara, Michael van der Heuvel et le docteur Claude Leroy déclarent n’avoir aucun lien d’intérêt financier avec le sujet évoqué dans l’article.
L’étude a été financée par Takeda Pharmaceutical Company Limited.
Cet article a été initiallement publié sur Medscape.de sous le titre KI erkennt Corona-Infektion am (erzwungenen) Husten – sogar bei asymptomatischen Patienten. Traduit et adapté par le Dr Claude Leroy.LIENS
Actualités Medscape © 2020 WebMD, LLC
Citer cet article: Coronavirus : une appli serait capable de repérer l’infection en analysant la toux – Medscape – 10 nov 2020.
FDA Clears Smartphone App to Interrupt PTSD-Related Nightmares

The US Food and Drug Administration has cleared for marketing a smartphone app that can detect and interrupt nightmares in adults with posttraumatic stress disorder (PTSD).
The NightWare app, from Minneapolis, Minnesota-based NightWare Inc runs on the Apple Watch and Apple iPhone.
During sleep, Apple Watch sensors monitor heart rate and body movement. These data are used to create a unique sleep profile using a proprietary algorithm.
When the NightWare app detects that a patient is experiencing a nightmare based on changes in heart rate and movement, it provides slight vibrations through the Apple Watch to arouse the patient and interrupt the nightmare, without fully awakening the patient, the company notes.
NightWare is available by prescription only and is intended for use in adults aged 22 years and older with PTSD.
“Sleep is an essential part of a person’s daily routine. However, certain adults who have a nightmare disorder or who experience nightmares from PTSD are not able to get the rest they need,” Carlos Peña, PhD, director, Office of Neurological and Physical Medicine Devices, Center for Devices and Radiological Health at FDA, said in a news release.
This authorization “offers a new, low-risk treatment option that uses digital technology in an effort to provide temporary relief from sleep disturbance related to nightmares,” said Peña.
NightWare was tested in a 30-day randomized, sham-controlled trial of 70 patients. Patients in the sham group wore the device, but no vibrations were provided.https://420b7a547e701c6e5f8246b5779ffca3.safeframe.googlesyndication.com/safeframe/1-0-37/html/container.html
Both the sham and active groups showed improvement in sleep on standard sleep scales, with the active group showing greater improvement than sham. “The evidence demonstrated the probable benefits outweighed the probable risks,” the FDA said in a statement.
NightWare is not a standalone therapy for PTSD and should be used in conjunction with prescribed medications for PTSD and other recommended therapies for PTSD-associated nightmares and nightmare disorder, the agency said.
NightWare was granted breakthrough device designation for the treatment of nightmares in patients with PTSD. The device reviewed through the de novo premarket pathway, a regulatory pathway for some low- to moderate-risk devices of a new type.
Along with this marketing authorization, the FDA is establishing “special controls” designed to provide a “reasonable assurance of safety and effectiveness for tests of this type,” the agency said.
Medscape Medical News © 2020
Cite this: Megan Brooks. FDA Clears Smartphone App to Interrupt PTSD-Related Nightmares – Medscape – Nov 09, 2020.
Nuevas tecnologías muestran resultados favorables en el tratamiento de lesiones pigmentadas

Los láseres de picosegundo y nanosegundo son mucho más eficaces para tratar lentigos individuales, en comparación con otros tipos de dispositivos, pero pulsos ultracortos conllevan más riesgo de hiperpigmentación posinflamatoria que la luz pulsada intensa o el láser de pulso prolongado, según el Dr. Mathew M. Avram, J. D.
Para tratar los melanosomas con fototermólisis selectiva, algunas longitudes de onda pico son 532 nm, 694 nm, 755 nm y 1.064 nm, señaló el Dr. Avram, director de Cirugía láser, estética y dermatológica en el Massachusetts General Hospital, en Boston, Estados Unidos, durante el Simposio Anual de Masters of Aesthetics, que se efectuó de manera virtual. “El objetivo ideal es una piel clara con una lesión pigmentada oscura. De esa forma se va a enfocar la energía en la melanina que está en la lesión en sí”, destacó.
Los láseres Q-switched y de picosegundo son eficaces para las lesiones pigmentadas. Utilizan tanta energía como la de la ciudad de Boston durante 20 – 30 mil millonésimas de segundo o 750 picosegundos. “Esto aumenta la temperatura a 1.000 ° C en ese instante, lo que produce el blanqueamiento epidérmico característico. Esta se dirige únicamente a las células pigmentarias, sean por pigmento exógeno o endógeno”, añadió.
Las lesiones pigmentadas benignas susceptibles al láser Q-switched de nanosegundo y de picosegundo son los lentigos y el nevo de Ota/Ito. El mecanismo de acción para el aclaramiento clínico consiste en la fragmentación y descarga de las células que contienen melanina, y la absorción y eliminación gradual de los fragmentos por macrófagos activados hacia los vasos linfáticos.
“Para obtener resultados efectivos no hay que memorizar a ciegas los ajustes, o reproducir los ajustes recomendados por un colega o un fabricante de un dispositivo”, recomendó el Dr. Avram, quien ejerció la jurisprudencia antes de su formación como médico.
“Algunos láseres no son calibrados de manera externa, por lo que se debe prestar atención al punto clínico final del láser, que en este caso es el blanqueamiento epidérmico. La ‘salpicadura’ de tejido es un punto clínico final inseguro y puede producir cicatrices. Los puntos clínicos finales seguros e inseguros del láser y la observación clínica estrecha son los mejores medios de evitar complicaciones y obtener los mejores resultados para los pacientes. El hallazgo clave es el punto clínico final, no los ajustes de la energía”.
Entre las lesiones pigmentadas que no se deben tratar con láser se encuentran nevos atípicos, lentigo maligno y otras formas de melanoma. “Cuando se tienen dudas hay que realizar una biopsia. Independientemente de quién remita el caso, uno es el responsable si trata un melanoma con un láser. Esto no es solo un diagnóstico incorrecto, sino probablemente también retrasa el diagnóstico. Si no se pueden reconocer las características morfológicas de la lesión pigmentada de base, no hay que tratarla. En algún momento esto va a ser contraproducente”, puntualizó.
Pacientes con más pigmento en la piel tienen mayor riesgo de hiperpigmentación posinflamatoria, continuó el especialista. Aunque los láseres pulsados más prolongados producen menos hiperpigmentación, también son menos eficaces para eliminar las lesiones. “Se puede combinar un láser pulsado prolongado con rejuvenecimiento fraccionado o luz pulsada intensa para optimizar la mejora. Si no se cuenta con dos láseres, se puede emplear solo uno pulsado más prolongado. El punto clínico final deseado del tratamiento con este enfoque es un aspecto gris ceniciento”, señaló. Las opciones son un láser de Nd:YAG de 532 nm con o sin enfriamiento, un láser de colorante pulsado de 595 nm sin enfriamiento, y un láser Alejandrita de 755-nm sin enfriamiento.https://tpc.googlesyndication.com/safeframe/1-0-37/html/container.html
Un avance en el tratamiento de las queratosis seborreicas es la estimulación con nanopulso , una nueva técnica que está desarrollando Pulse Biosciences.[1] Con esta técnica los pulsos de energía eléctrica durante nanosegundos producen alteración de los orgánulos internos, lo que conduce a muerte celular regulada. “El efecto específico en la célula es no térmico, ya que un nanopulso característico libera 0,1 J de energía distribuida en un volumen de tejido”, indicó el Dr. Avram.
Estudios humanos en fase temprana establecieron las dosis seguras y la validación de las hipótesis sobre los mecanismos para la eficacia en lesiones benignas. “Lo que se tiene son pequeñísimos nanoporos que permiten que los iones de calcio fluyan hacia la célula”.
“Los nanoporos en el retículo endoplásmico permiten que los iones de calcio fluyan afuera del retículo endoplásmico y lo estresen. Estos nanoporos en las mitocondrias alteran la capacidad para generar energía, y la célula muere”, puntualizó.
Los estudios histológicos han revelado que al cabo de días el procedimiento produce muerte celular regulada sin efectos térmicos. La capacidad de la energía de estimulación con nanopulso para despejar queratosis seborreicas se confirmó en un estudio de 58 individuos en el que se trataron 174 lesiones de queratosis seborreicas.[3] La mayor parte de estas (82%) se clasificó como claras o mayormente claras 106 días después del tratamiento. Los resultados reflejaron una sola sesión de tratamiento.
Otro nuevo tratamiento, la “criomodulación”, una tecnología desarrollada por el Dr. R. Rox Anderson, el Dr. Dieter Manstein, Ph. D. y el Dr. Henry Chan, Ph. D., expresa el cambio en la piel inducido por el frío como una manera de detener la producción de melanina.[4] El Dr. Avram explicó: “Se logra detener la producción de melanina pero se conserva la función del melanocito. Hay una barrera epidérmica normal y no hay respuesta inflamatoria persistente, por lo que no ocurre hiperpigmentación”.
Caracterizó a la criomodulación como un procedimiento clínico fácil de utilizar para tratar lesiones benignas en todos los tipos de piel. Se aplica una mascarilla para confinar el congelamiento al área de tratamiento deseada, y se utiliza gasa hidratada para facilitar la propagación de los cristales de hielo.
Un prototipo del dispositivo presenta una selección de parámetros basados en el tipo de lesión, la ubicación anatómica y el tipo de piel. “Utiliza entre 107 y 166 kJ/m2 de energía extraída, y se toman fotos al inicio y en el seguimiento. Durante dos a tres días hay eritema, oscurecimiento y edema. Es bien tolerado, con molestia mínima. No hay discromía a largo plazo. Esto es agradable, pues los pacientes tienen poco o nulo tiempo de inactividad”, finalizó el especialista.
El Dr. Avram declaró que ha recibido honorarios por consultoría de Allergan, Merz, Sciton y Soliton. También informó tener acciones o participación accionarial en Cytrellis.
Este artículo fue publicado originalmente en MDedge.com, parte de la Red Profesional de Medscape.
Medscape © 2020 WebMD, LLC
Cualesquiera puntos de vista expresados antes son del propio autor y no necesariamente reflejan los puntos de vista de WebMd o Medscape.
Citar este artículo: Nuevas tecnologías muestran resultados favorables en el tratamiento de lesiones pigmentadas – Medscape – 22 de oct de 2020.